In a rare medical case, a 32-year-old Lebanese woman experienced a severe heart attack, known as ST elevation myocardial infarction (STEMI), attributed to massive coronary artery thrombosis. This incident occurred eight months after she began using oral contraceptive pills (OCPs), despite having no traditional cardiovascular risk factors. The case highlights potential risks associated with OCPs, even among young, healthy women.
The patient presented with progressive chest pain and severe left arm pain, accompanied by nausea and vomiting. Her medical history was unremarkable, with no hypertension, diabetes, or dyslipidemia, and she had no family history of heart disease. The patient had been taking Yasmin, a common OCP, for the past eight months.
Understanding Coronary Thrombosis and OCPs
Coronary artery thrombosis is a serious condition that can lead to significant morbidity and mortality. It is more commonly associated with older generations of OCPs and traditional risk factors like hypertension and diabetes. However, recent studies suggest that thrombosis can occur without these risk factors, as seen in this case.
Earlier research, including works by Maleki and Lange, and more recent studies by Pertuz et al., indicate a complex relationship between OCPs and coronary thrombosis. Rahhal et al. noted that modern OCP formulations, with reduced estrogen doses, have decreased the incidence of coronary thromboembolism. Despite this, there remains a lack of studies on coronary thromboembolism from nonatherosclerotic causes.
Case Details and Medical Response
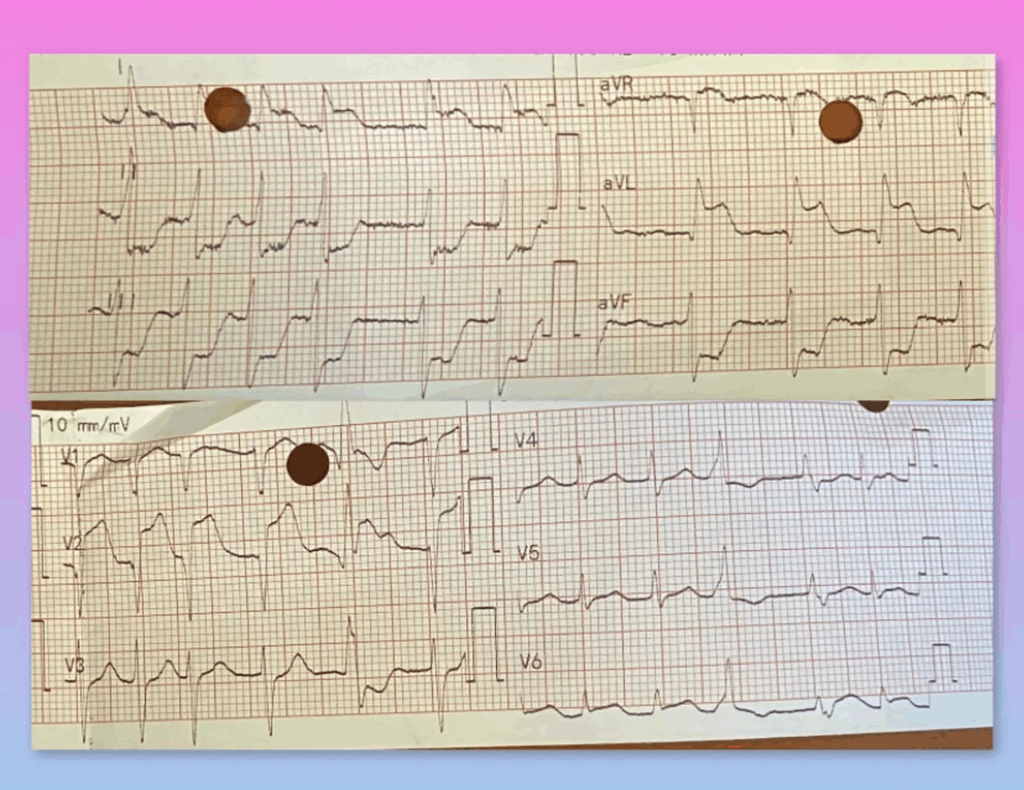
Upon examination, the patient showed sinus tachycardia and mild hypotension. An electrocardiogram revealed significant ST segment elevation, and lab tests indicated elevated troponin levels. Echocardiography showed wall akinesia in the left ventricle.
Diagnosed with STEMI, the patient received immediate treatment, including ticagrelor, aspirin, atorvastatin, and heparin, before undergoing cardiac catheterization. Coronary angiography revealed a massive thrombus in the left main coronary artery, which was treated with a drug-eluting stent.
Broader Implications of OCP Use
OCPs are among the most widely used contraceptives globally and have undergone significant changes since their introduction. Modern formulations have reduced estrogen doses to mitigate thrombotic risks. Despite these advancements, the cardiovascular safety of OCPs remains a concern.
Research has shown that OCPs can increase clotting factors and reduce natural anticoagulants, contributing to thrombotic risks. High estrogen doses are linked to arterial thrombotic risks, while newer OCPs pose a higher risk of arterial thromboembolism compared to earlier versions.
Studies indicate that OCPs increase the risk of arterial thrombosis by 1.6-fold, with higher estrogen doses doubling this risk.
Conflicting Evidence and Ongoing Research
Research on the risk of arterial thrombosis with different OCP types has yielded mixed results. A Cochrane meta-analysis found no significant risk difference based on progestin type, but higher estrogen doses were associated with increased thrombosis risk. A Danish study supported these findings, showing increased myocardial infarction risk with higher estrogen doses.
Further studies, such as those by Karabay et al., have explored the link between specific OCP brands like Yasmin and thrombus burden. Case reports have documented similar incidents of coronary thrombosis in women without traditional risk factors.
Conclusion and Future Directions
This case underscores the need for healthcare providers to be aware of the potential cardiovascular risks associated with OCPs, even in patients without traditional risk factors. It highlights the importance of ongoing research to better understand the relationship between OCPs and cardiovascular events.
As OCPs continue to evolve, it is crucial to monitor their effects on cardiovascular health and to educate patients about potential risks. This case serves as a reminder of the complexities involved in prescribing and using OCPs, emphasizing the need for personalized healthcare approaches.







