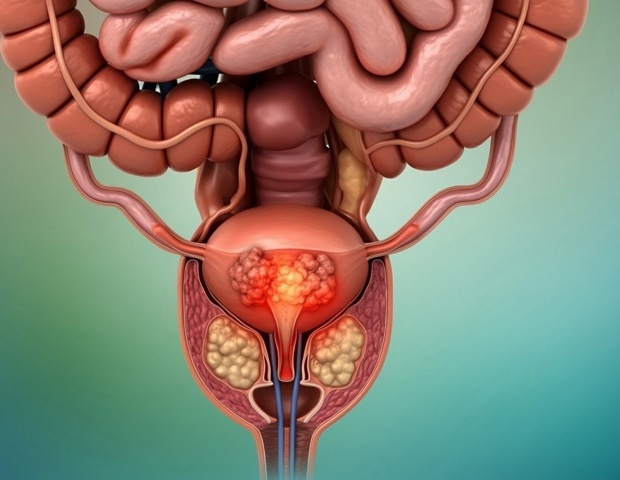
Current prostate-specific antigen (PSA) testing practices may not effectively target those most likely to benefit, raising concerns about overtesting, warn researchers from the University of Oxford. Their study, published in The BMJ, analyzed data from over 10 million men across England.
Despite UK guidelines recommending PSA testing only for symptomatic patients or after consultation with a general practitioner, the study reveals that many men undergo frequent testing without symptoms. This includes repeat testing in patients with previously low PSA values, indicating a potential overuse of the test.
Understanding PSA Testing Patterns
The study aimed to shed light on how PSA tests are utilized in primary care settings across England. Researchers examined data from 10,235,805 men aged 18 and over, registered at 1,442 general practices between 2000 and 2018, who had no prior prostate cancer diagnosis.
Data were meticulously linked to the National Cancer Registry, Hospital Episode Statistics, and the Office for National Statistics. The analysis considered various factors, including region, socioeconomic status, age, ethnicity, family history of prostate cancer, symptom presentation, and PSA values.
“A total of 1,521,116 men had at least one PSA test during the study period, resulting in 3,835,440 PSA tests overall.”
Testing increased fivefold over the study period, particularly among men without symptoms and those with PSA values below recommended thresholds. The highest testing rates were observed in men aged 70 and older, who are least likely to benefit from repeat testing, and in much younger men, aged 18-39, than typically recommended.
Regional and Demographic Variations
Testing rates varied significantly by region, socioeconomic status, ethnicity, family history, age, PSA value, and symptoms. The highest rates were seen among patients of white ethnicity and those from less deprived areas.
“Almost half of the men (735,750) were retested. Of these, more than 75% had no symptoms recorded, and 73% never had a PSA value above the recommended threshold.”
The average interval between tests was just over 12 months overall, and 17 months for patients who never exceeded the recommended PSA threshold. This interval is shorter than most guidelines suggest. Patients were retested more frequently if they were older, belonged to non-white ethnic groups, had a family history of prostate cancer, or had previously elevated PSA values.
Implications and Calls for Action
The researchers acknowledge the limitations of using routinely collected primary care data, noting potential biases in their analyses. However, they assert that their findings are robust and highlight the variability in PSA testing practices.
“PSA testing in primary care is varied. Among patients who underwent multiple tests, many were tested more frequently than recommended, raising concerns about overtesting,” the authors conclude.
They emphasize the urgent need for research to establish appropriate, evidence-based PSA retesting intervals to maximize patient benefit while minimizing the risks of overtesting.
Expert Opinions and Future Directions
Dr. Juan Franco and colleagues, in a linked editorial, express concerns that unregulated PSA testing could lead to significant costs and harm, potentially increasing the incidence of undetected prostate cancer while failing to identify cases most likely to cause symptoms and death.
They welcome the European Commission’s interest in population-based cancer screening, including for prostate cancer, but stress the importance of grounding these efforts in high-quality evidence from randomized trials.
“This study highlights the need for better NICE guidance, especially in men outside of recommended ages or men with lower urinary tract symptoms, erectile dysfunction, or other conditions unrelated to prostate cancer,” they conclude.
The findings underscore the necessity for consistent international guidelines and a more nuanced approach to PSA testing, ensuring that it serves as a beneficial tool rather than a source of unnecessary anxiety and medical intervention.