Deep brain stimulation (DBS) of the subthalamic nucleus (STN) has long been recognized as a transformative treatment for advanced Parkinson’s disease (PD), particularly for its ability to alleviate motor symptoms. However, the subjective perceptions of DBS outcomes among patients, caregivers, and neurologists remain less understood. A recent study sheds light on these perspectives, offering valuable insights into the multifaceted impacts of DBS.
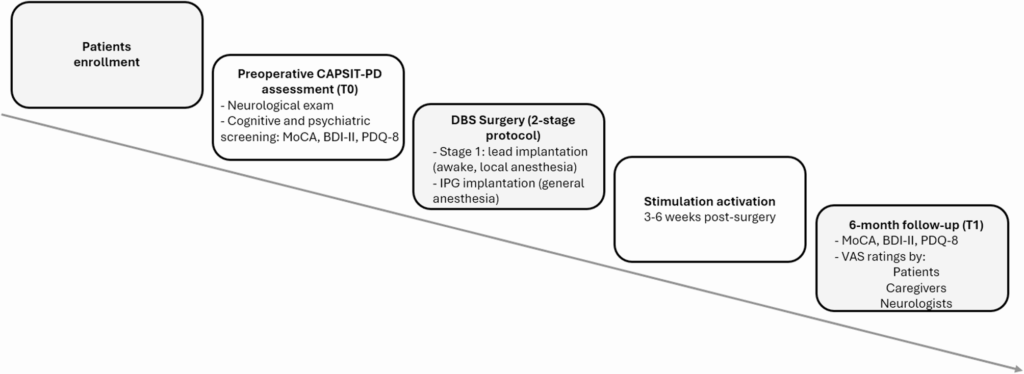
The study involved 25 PD patients who underwent bilateral STN-DBS, along with their caregivers and neurologists. Six months post-surgery, participants rated perceived psychological and physical improvements using Visual Analogue Scales (VAS). The findings revealed an average improvement of 60% in the psychological domain and over 75% in the physical domain, with no significant differences between the groups.
Exploring the Subjective Experience
Parkinson’s disease, a progressive neurodegenerative disorder, is primarily managed through pharmacological treatments. However, after several years of medication, many patients face drug-related motor complications. DBS has emerged as a crucial intervention, reducing “off” time and improving both motor and non-motor symptoms. Yet, the journey with DBS is not solely about motor improvements.
As the study highlights, the subjective experience of patients post-DBS is complex. While objective motor improvements are well-documented, personal and socio-professional adjustments can pose challenges. The decision to undergo DBS is significant, requiring careful consideration of potential benefits and risks. Capturing patients’ experiences is essential for a comprehensive treatment assessment.
Perception Gaps and Agreement
The study aimed to investigate the perception gap between patients, caregivers, and neurologists regarding DBS outcomes. Interestingly, the agreement rate among these groups was moderate-to-good, indicating consistency in perceived improvements. This alignment suggests that patient self-reports are reliable, reinforcing the importance of integrating these reports into treatment assessments.
“Patients, caregivers, and neurologists consistently perceived a positive impact of DBS, particularly in the physical domain,” the study noted.
Despite the overall agreement, the study found that psychological improvements were rated lower than physical ones, highlighting the persistence of non-motor symptoms like mood and anxiety issues. This nuance underscores the importance of addressing both motor and non-motor outcomes in PD treatment.
Implications for Patient-Centered Care
The findings have significant implications for patient-centered care. By understanding the subjective perceptions of DBS, healthcare providers can tailor interventions to better meet the needs of patients. The study also emphasizes the value of proxy assessments from caregivers and neurologists, which complement patient-reported outcomes.
Notably, the study found no significant associations between perceived improvements and most clinical or demographic variables, suggesting that subjective perceptions are largely independent of these factors. However, the limited sample size calls for further research to confirm these observations.
Future Directions and Considerations
This study marks a step forward in understanding the subjective outcomes of DBS in PD. Future research should explore factors influencing perceptions over time, including preoperative expectations and clinical characteristics. A longitudinal approach could provide deeper insights into how perceptions evolve and the role of proxy assessments in long-term care.
Ultimately, the study underscores the importance of a multidimensional approach to DBS outcome assessment, integrating patient-reported outcomes with clinical measures. Such an approach not only enhances the understanding of DBS impacts but also supports the development of personalized treatment strategies and rehabilitation protocols.
As the landscape of PD treatment continues to evolve, studies like this play a crucial role in shaping patient-centered care, ensuring that interventions align with the diverse needs and experiences of those living with Parkinson’s disease.