Autoimmune diseases arise from a complex interplay of immune dysregulation, marked by chronic inflammation and a loss of self-tolerance. Central to these processes are cytokines, the soluble signaling proteins that orchestrate immune responses by mediating intercellular communication.
Cytokine networks display dual functionality. While they are crucial regulators of immune homeostasis, they paradoxically act as pathogenic drivers in diseases such as systemic lupus erythematosus (SLE), psoriasis, rheumatoid arthritis (RA), and inflammatory myopathies. Recent research has underscored the therapeutic potential of cytokine-targeted biologics, Janus kinase (JAK) inhibitors, and emerging strategies like engineered cytokines and miRNA modulation.
Mechanisms of Autoimmunity
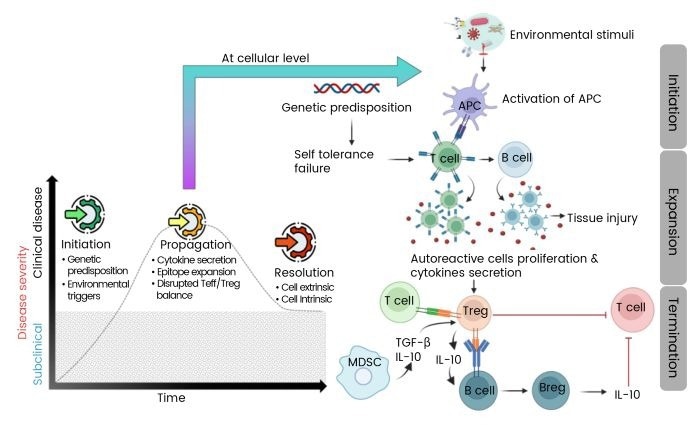
Autoimmunity results from complex disruptions in immune signaling pathways, leading to tissue damage. Genetic predisposition and environmental factors can trigger excessive cytokine production, activation of self-reactive lymphocytes, and autoantibody release. Resolution of autoimmune processes is sometimes possible by restoring regulatory mechanisms through regulatory T cells (Tregs) and regulatory B cells (Bregs), which produce immunosuppressive cytokines like interleukin-10 (IL-10) and transforming growth factor-beta (TGF-β).
“Restoring immune equilibrium is key to resolving autoimmune processes,” says Dr. Jane Doe, an immunologist at the National Institute of Health.
Cytokine Networks in Autoimmune Pathogenesis
Autoimmune diseases are often driven by a hyperactive pro-inflammatory cytokine environment. For instance, IL-6, IL-17, and tumor necrosis factor-alpha (TNF-α) are core mediators in conditions like psoriasis and RA. The IL-1 family, including IL-1β and IL-18, exacerbates tissue damage by activating the NLRP3 inflammasome, a mechanism implicated in SLE.
“Pro-inflammatory cytokines not only drive local inflammation but also contribute to systemic manifestations like fatigue and fever,” explains Dr. John Smith, a rheumatologist at Johns Hopkins University.
Regulatory Cytokine Deficiencies
Immunosuppressive cytokines such as IL-10 and TGF-β play protective roles by counterbalancing pro-inflammatory signals. Reduced IL-10 production by Bregs has been associated with disease flares in SLE, highlighting its protective role. TGF-β maintains peripheral tolerance by suppressing effector T cell proliferation and inducing Treg differentiation.
Dysregulation of these pathways creates a permissive environment for autoimmunity, observable in RA and multiple sclerosis (MS), where defective TGF-β signaling permits unchecked Th17 activity.
Therapeutic Targeting of Cytokine Networks
Biologic Therapies
Biologic therapies have transformed the treatment landscape for autoimmune diseases. Anti-TNF-α agents, such as adalimumab and infliximab, have significantly reduced synovitis and radiographic progression in RA. However, TNF blockade can induce psoriasiform lesions in some patients, underscoring cytokine pleiotropy.
IL-6 inhibition with Tocilizumab has shown efficacy in ameliorating systemic inflammation in juvenile idiopathic arthritis (JIA) and RA. Similarly, IL-17/IL-23 axis targeting with drugs like Secukinumab and Ustekinumab has achieved rapid skin clearance in psoriasis.
JAK/STAT Inhibition
JAK inhibitors, such as Tofacitinib and Baricitinib, block downstream STAT phosphorylation, effectively modulating cytokine signaling. These inhibitors are approved for RA treatment and have shown promise in reducing IFN-α signature and ameliorating nephritis in SLE.
Innovative Approaches
Emerging strategies include IL-2-based immunotherapies, which expand Tregs to restore immune tolerance, and miRNA modulation, which regulates cytokine production post-transcriptionally. Engineered cytokines, such as PEGylated IL-10, offer promising new strategies for fibrosis-prone diseases like systemic sclerosis.
“The integration of mechanistic insights with innovative therapeutics is set to open up the next frontier in autoimmunity,” notes Dr. Emily White, a leading researcher in cytokine biology.
Challenges and Future Directions
Pioneering developments in cytokine biology have enabled precision therapies targeting key nodes within cytokine networks. However, challenges such as pleiotropy, interpatient heterogeneity, and cytokine redundancy remain. Future research directions include personalized cytokine profiling, microbiome-directed interventions, and engineered biologics with enhanced cell-type specificity.
Sino Biological plays a key role in advancing early detection and targeted therapy development for autoimmune diseases by providing high-quality tools for biomarker analysis and drug discovery. Their comprehensive portfolio includes cytokines, kinases, and target proteins, essential for advancing autoimmune research.
As the understanding of cytokine networks deepens, the potential for novel therapeutic interventions grows, promising a new era in the treatment of autoimmune diseases.