Dawn had just broken across the trail through the Pir Panjal mountains when Fatima Deader felt the first labor pains. She and her family were nearing the midway point of their 134-mile trek from Rajouri in Jammu to Kashmir’s higher pastures. Mist clung to the forest, and the ground was slick beneath the feet of the caravan of about 70 pastoralists who had camped together the previous night.
A week from her due date, Fatima had been traveling on horseback, assuming the discomfort she felt was fatigue—until pain tore through her body. “There was no clinic, no nurse, no doctor,” Fatima, 23, recounts. Only her mother and a midwife, Saira Begum, were with her in a damp canvas tent, whispering prayers. Hours after her son was born, still weak and bleeding, she had to ride again, her baby carefully tied to the horse with her, as the group’s journey continued through dense forest, home to tigers and bears.
The Journey of Nomadic Herders
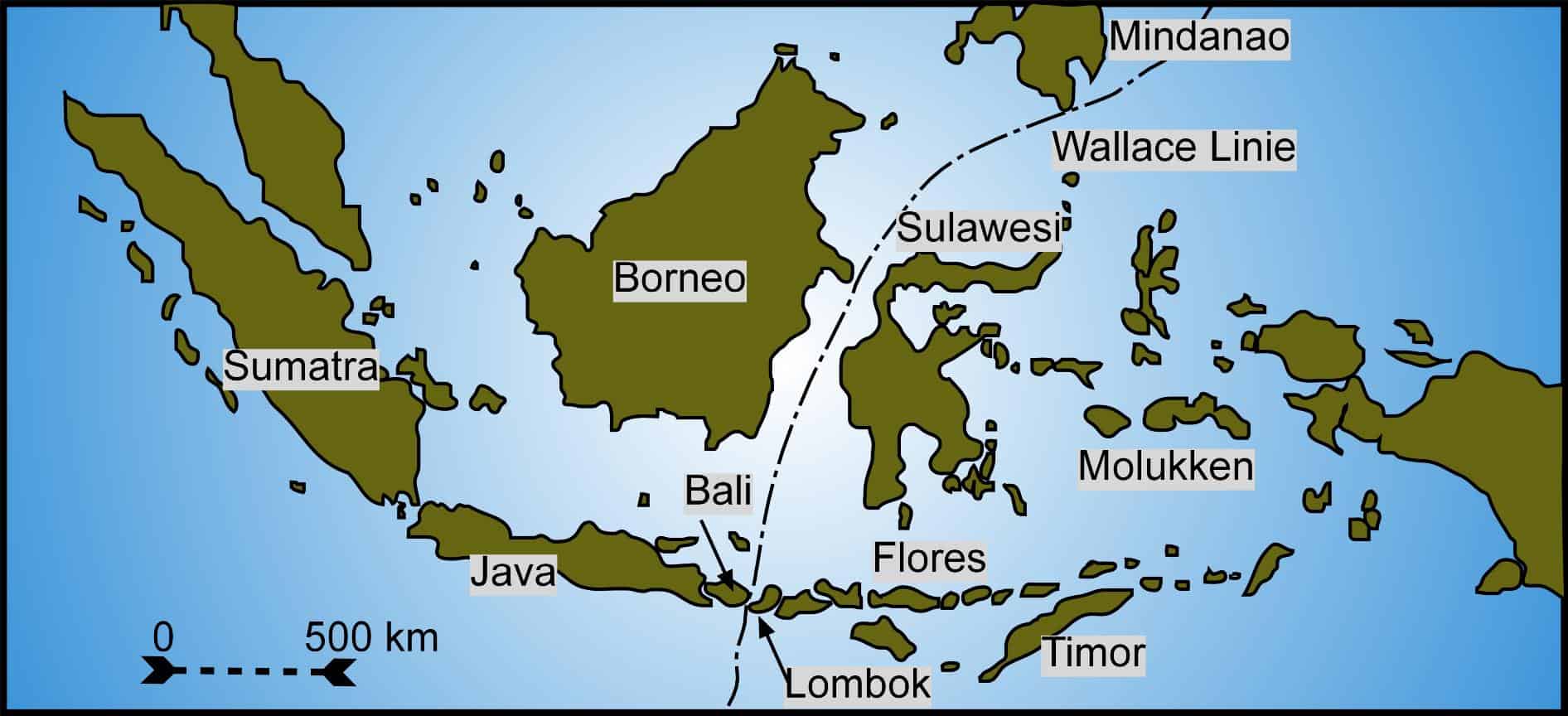
The 3,500-meter-high Pir Panjal pass, also known as Peer Ki Gali, connects the Jammu region to the Kashmir valley via the centuries-old Mughal Road. Each year, when the snow melts, nearly a million nomadic Gujjar and Bakarwal herders set out with their goats, sheep, and horses on journeys that can last months. For those pregnant during the migration, heavy loads still have to be carried, and rest found in tents pitched on wet ground. Babies are born under trees, by riverbanks, or in forest shelters.
Some women give birth after days without a proper meal. Those who make it to district hospitals often arrive exhausted, anemic, or suffering from an infection. Fozia Choudhary was 16 when she gave birth in 2016. “I was still a child myself,” she says. Married to her cousin at 14—early marriage is common among tribal families—she often had nothing to eat but a cup of milk and a single roti flatbread each day. By the time she went into labor, she was dangerously weak.
“They shouted at my husband, asking how I had even survived this long,” Choudhary recalls.
Challenges in Healthcare Access
For women like Choudhary, survival often depends on traditional midwives. At 63, Begum has helped deliver dozens of babies along the mountain routes. “Sometimes there is so much blood loss we can’t save the mother,” she says, recalling a tragic incident in Doodhpathri in 2021 where a woman died due to lack of medical aid.
A 2022 government study estimated Jammu and Kashmir’s maternal mortality ratio (MMR) to be 46, better than India’s national figure and well below the global average of 224 deaths. However, these numbers obscure the experiences of nomadic women, whose lives largely go undocumented in official health data.
Dr. Mushtaq Wani, a public health researcher in Srinagar, notes, “The state’s MMR figures come from hospital deliveries. Women on migration routes rarely reach clinics in time, so preventable deaths go unrecorded.”
Kashmiri political leader Yasin Malik highlights that for decades, successive administrations have promised mobile healthcare for Gujjar and Bakarwal women, but support has never materialized. A senior Jammu and Kashmir government health official, who wished to remain anonymous, admitted that staffing, funding, and the terrain made medical support difficult.
Global Parallels and Potential Solutions
The gap in healthcare is compounded by poverty, early marriage, and malnutrition. Many women, particularly those who married young, enter pregnancy undernourished and physically underdeveloped, increasing the risk of maternal and neonatal complications. International organizations note that this issue is not unique to the region.
The UN Population Fund (UNFPA) observes similar patterns among pastoralist women in other countries where migration routes leave those facing childbirth out of reach of conventional healthcare.
Pilot projects in countries like Mongolia, Ethiopia, and Somalia have attempted to address the lack of resources for nomadic women. In Mongolia, an outreach initiative using mobile clinics, supported by the World Health Organization (WHO), provides preventive care and ultrasound scans to herders in remote areas. Ethiopia’s mobile health program delivers antenatal, immunization, and nutrition services to hard-to-reach pastoralist communities through traveling health teams.
Back in the forest, Begum folds her cloths after helping another young woman deliver her baby. “What else do you have in the jungles, except an old woman’s hands?” she asks. The new mother, Fatima, rocks her newborn by the glow of a fire, echoing her sentiment. “We survive by luck,” she says. “But every year, another woman does not.”
The stories of these women highlight a pressing need for targeted healthcare solutions that can traverse the challenging terrains and reach the most vulnerable. As the world continues to grapple with healthcare inequities, the resilience and courage of these women serve as a poignant reminder of the work still to be done.