Mice pups conceived through in vitro fertilization (IVF) in laboratory settings exhibit slightly higher rates of DNA mutations compared to those conceived naturally, according to a recent study on artificial reproductive technologies. The research, published in the journal Genome Research, underscores the need to understand how fertility treatments might impact the DNA of offspring, although the findings cannot be directly applied to humans.
The study was led by Beth Dumont, a geneticist at The Jackson Laboratory. “What we are seeing is a true biological signal, but we cannot make an apples-to-apples comparison relative to what happens in a clinic. Still, the fact that we see this trend in mice does argue for additional research investigating this possibility in humans,” Dumont stated.
Comparative Analysis of Genetic Mutations
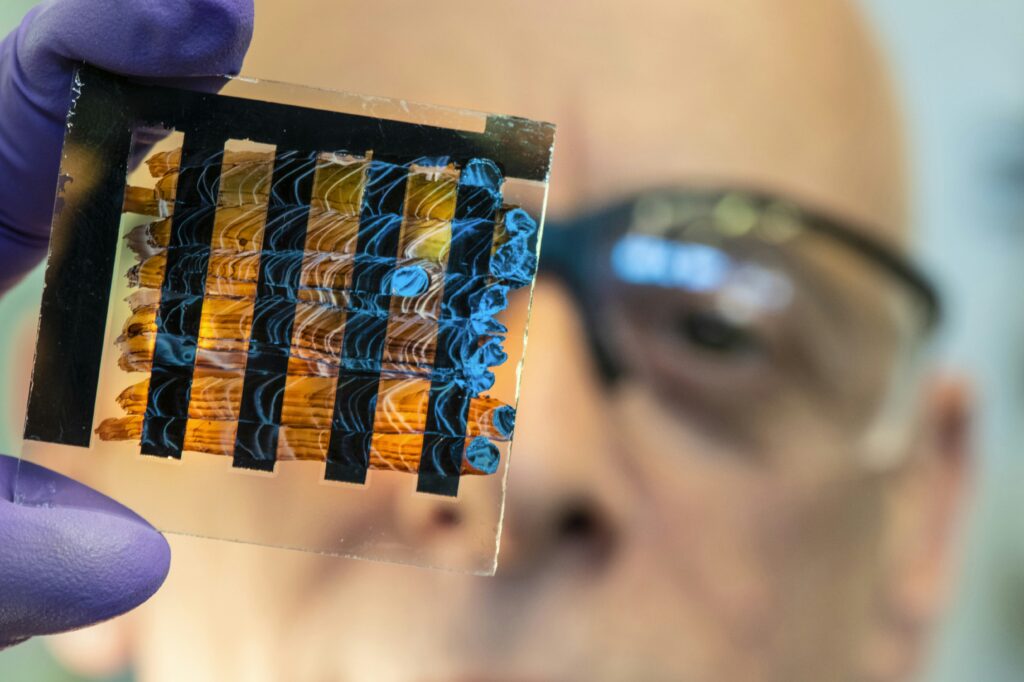
The research team conducted a comparative analysis of genome sequences from lab mice conceived naturally and those conceived through assisted reproductive technologies, including hormone treatments, IVF, and embryo transfer. The results showed that pups born through these fertility treatments had approximately 30% more new single-nucleotide variants, or minor changes in DNA sequences.
Nucleotides, the building blocks of DNA, are arranged in specific sequences that serve as instructions for cellular growth and function. Single-nucleotide variants represent genetic differences involving a change in just one DNA letter, which can occur during DNA replication. Despite the increase in mutation rates, the study suggests these mutations are unlikely to be harmful.
Scientists estimate that fewer than 2% of new mutations arising in a genome are deleterious or have an impact on an individual’s phenotype or disease susceptibility.
Implications of Increased Mutation Rates
The mutations observed in the study were distributed across the genome rather than concentrated in specific genes. The timing of these mutations in early embryos appeared similar between fertility-treated and natural groups, suggesting that while fertility treatments may increase the overall chance of new DNA changes, they do not affect the timing of these changes during development.
“Even though we see an increase in mutation rate, most of these mutations are peppered across the genome, and they are neutral mutations that have no impact overall on the organism’s phenotype,” Dumont explained. “Because it’s not a huge leap in mutation rate, the risk that any one of those new mutations would be deleterious is really, really small—almost negligible.”
Even with a 30% increase in new mutations, the absolute number of harmful new mutations per mouse remains low. For every 50 mice conceived with IVF, scientists expect roughly one additional harmful DNA change compared to natural conception. This effect is akin to the impact of a 30-week increase in the male parent’s age, a known factor in mutation rates among mammals.
Unraveling the Biological Mechanisms
The biological mechanisms behind these genetic changes remain unclear. Further research is necessary to determine whether the new mutations stem from a specific step in the IVF process or the combined effects of several steps. Hormone treatments that stimulate the ovaries, for instance, might contribute to these mutations since they push eggs to restart meiosis, a cell division stage prone to errors. Other factors, such as the physical handling of embryos or the chemical conditions of lab environments, could also play a role.
While the study does not confirm whether the same effects occur in humans, it raises important questions. Fertility procedures differ between mice and humans, and their reproductive biology varies significantly. For instance, mice do not menstruate, and humans undergoing IVF may encounter environmental factors that could have already influenced their genetics.
“Nothing in our study directly speaks to the potential of mutations in human IVF, but there have been associations in the literature suggesting some steps in IVF might induce genetic changes. That is clearly worth studying to ensure patients are maximally informed,” Dumont said.
The study’s authors include Laura Blanco-Berdugo and Alexis Garretson of The Jackson Laboratory. The research received support from start-up funds provided by The Jackson Laboratory and a Maximizing Investigators’ Research Award from The National Institute of General Medical Sciences (R35 GM133415).
The findings highlight the need for continued exploration into the genetic implications of fertility treatments, not only in mice but potentially in humans as well. As artificial reproductive technologies advance, understanding their impact on genetic integrity remains a critical area of study.