A groundbreaking study co-authored by UCLA Health researchers has uncovered that nearly nine in ten emergency department patients in the United States have not received one or more recommended vaccines. Alarmingly, about half of these individuals were unaware that these vaccines were even recommended for them. The study highlights significant gaps in preventive care, particularly among underserved populations who rely on emergency departments as their primary healthcare access point.
The findings underscore the urgent need to address these gaps, especially considering that approximately 30% of the U.S. population lacks access to primary care and depends solely on emergency departments for healthcare. This demographic includes uninsured individuals, many homeless people, and immigrants, all of whom often fall through the cracks of traditional healthcare systems. Vaccines, known for saving more lives than almost any other public health intervention, must be made more accessible to these communities to improve public health outcomes.
Comprehensive National Study in Emergency Departments
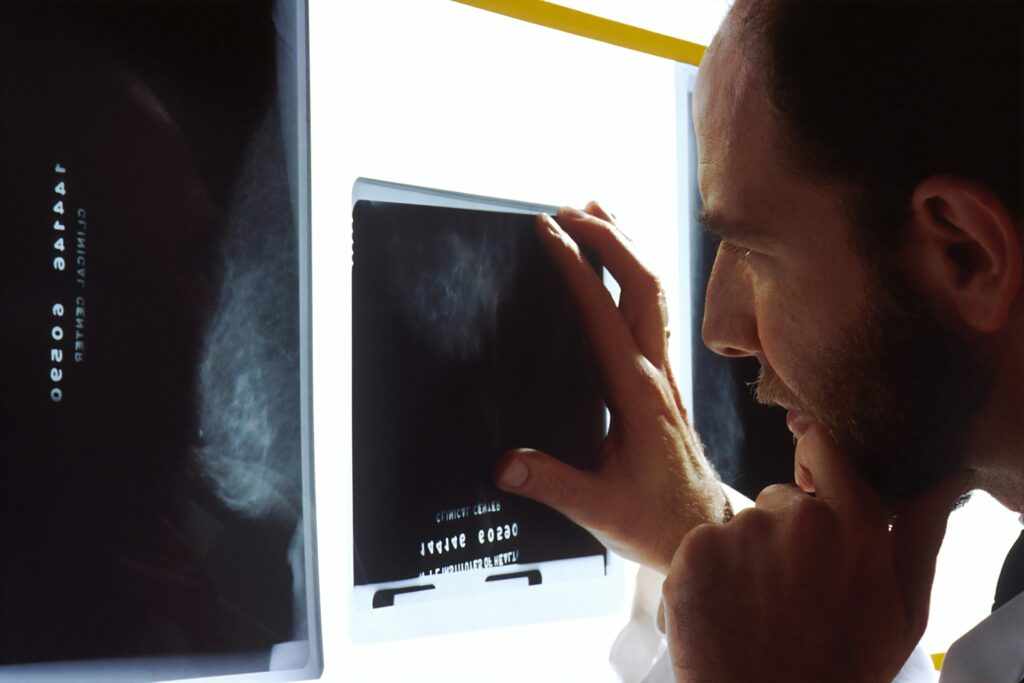
The research represents the first national comprehensive vaccine surveillance study conducted in emergency departments across eight U.S. cities. Between April and December 2024, researchers surveyed 3,285 non-critically ill adult patients visiting 10 emergency departments for minor injuries or illnesses. The survey included age-specific questions about vaccines such as shingles, pneumococcal, RSV, tetanus, COVID-19, and influenza. Patients were asked if they had heard of these vaccines, whether they had received them, and if not, why. Additionally, they were queried on their willingness to accept vaccines if offered during their emergency department visit.
Key Findings and Implications
The study found that nearly 86% of emergency department patients had not received one or more recommended vaccines, and about 49% were unaware of the vaccines recommended for them. Lack of vaccination was notably higher among African Americans, uninsured individuals, and those without a primary care provider. Interestingly, roughly half of the unvaccinated participants expressed willingness to accept vaccines if offered during their emergency department visit, indicating a significant opportunity for improvement.
“Currently, only 14% of adult ED patients are fully up-to-date on their vaccines. If implemented widely, ED-based vaccine programs could increase fully vaccinated rates to as high as 48%, more than tripling current rates.”
Future Directions and Potential Solutions
In response to these findings, researchers are exploring ways to automate the vaccination screening process to reduce the labor-intensive burden on emergency departments. They are also investigating mobile outreach options for individuals unable to access emergency departments. The team advocates for collaborations between public health officials and emergency department personnel to develop effective programs for vaccine screening, outreach, and delivery.
Expert Insights
Dr. Jesus R. Torres, assistant professor in the UCLA Department of Emergency Medicine at the David Geffen School of Medicine and study co-author, emphasized the importance of emergency departments as a critical touchpoint for reaching patients who might otherwise never encounter the healthcare system for preventive care.
“Our findings demonstrate that ED-based vaccination programs could serve as a powerful tool for advancing health equity, particularly for communities that have been historically underserved by traditional healthcare delivery models,” said Dr. Torres.
About the Study and Research Team
The study, titled “Emergency Department Survey of Vaccination Knowledge, Vaccination Coverage, and Willingness to Receive Vaccines in an Emergency Department Among Underserved Populations — Eight U.S. Cities, April–December, 2024,” was published in the MMWR Morb Mortal Wkly Rep 2025. It was led by Dr. Robert Rodriguez at UC Riverside, with contributions from colleagues at UCLA, UC San Francisco, Thomas Jefferson University in Pennsylvania, Wayne State University in Michigan, Rush University Medical Center in Illinois, and Duke University in North Carolina. The study was partially funded by a grant from the National Institute of Allergy and Infectious Diseases.
This research highlights a critical opportunity to improve public health by leveraging emergency departments as venues for vaccine delivery, thereby addressing the healthcare access disparities faced by underserved populations. As the study progresses, it could pave the way for innovative approaches to preventive care in the United States.