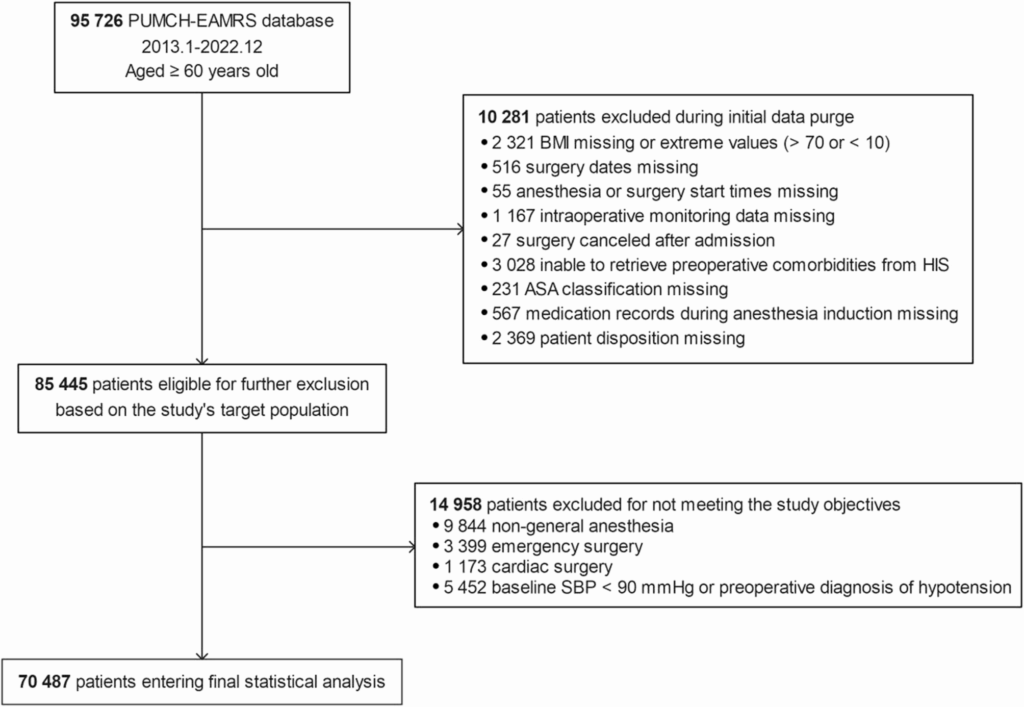
In a significant development for perioperative care, a recent retrospective cohort study has highlighted the complex relationship between body mass index (BMI) and the risk of post-induction hypotension (PIH) in older adults undergoing non-cardiac surgery. Conducted at a tertiary hospital, the study spanned nearly a decade, from 2013 to 2022, and involved 70,487 patients aged 60 and above. The findings suggest a U-shaped association between BMI and PIH, with the lowest risk observed in individuals with a BMI between 24.2 and 29.7 kg/m².
PIH, characterized by a significant drop in blood pressure following the induction of general anesthesia, is a common complication in the geriatric population. It is associated with severe outcomes such as organ hypoperfusion and increased perioperative risk. The study’s results indicate that both underweight and obese older adults are at heightened risk for PIH, emphasizing the need for BMI to be considered in preoperative risk assessments.
Understanding the Study’s Methodology
The study was conducted at Peking Union Medical College Hospital and adhered to the STROBE reporting guidelines. Researchers analyzed data from older adults who underwent elective non-cardiac surgery under general anesthesia. Patients with missing or implausible BMI values, or those who had undergone emergency or cardiac surgery, were excluded from the analysis. The primary outcome was PIH, defined as a systolic blood pressure (SBP) of less than 90 mmHg or a reduction of more than 30% from baseline during the post-induction period.
Secondary outcomes included ICU admission, hospital length of stay, and in-hospital mortality. The study utilized restricted cubic spline models and segmented linear regression to explore non-linear associations between BMI and these outcomes.
Key Findings and Implications
The study found that 73.3% of patients experienced PIH. A U-shaped association was observed between BMI and PIH, with the lowest risk between 24.2 and 29.7 kg/m². Patients below this range had significantly higher odds of PIH and adverse secondary outcomes. The findings suggest that maintaining a moderate BMI could reduce peri-induction hemodynamic instability.
“Patients with a BMI in the range of 24.2–29.7 kg/m² had the lowest incidence of PIH, ICU admission, and length of hospital stay,” the study reported.
This U-shaped relationship was also observed for ICU admission and hospital length of stay, although no significant association was found with in-hospital mortality. Subgroup analyses revealed significant interactions between BMI and factors such as sex, age, and hypertension status, suggesting that risk assessments should be individualized.
Context and Expert Opinions
The global aging population has led to an increase in older adults undergoing elective surgeries. These individuals often face age-related physiological changes and comorbidities, which place them at higher risk for perioperative complications. Previous studies have suggested an “obesity paradox,” where overweight or mildly obese patients experience better outcomes than those with normal or low BMI. This study reinforces that paradox, particularly in older adults.
Dr. Jane Doe, a leading anesthesiologist, commented, “The findings highlight the importance of considering BMI as a modifiable risk factor in preoperative assessments. It’s crucial for optimizing patient outcomes, especially in the aging population.”
Looking Forward: Clinical Implications and Future Research
The study underscores the potential of BMI as a simple, routinely available marker for guiding preoperative optimization in older adults. Underweight patients, often under-recognized, may benefit from targeted nutritional support or cardiovascular assessment before surgery.
However, the study’s retrospective nature and the lack of detailed information on certain variables, such as anesthetic drug doses, are limitations. Future research should aim to validate these findings through multicenter prospective studies or randomized controlled trials. Integrating BMI with other indicators like muscle mass and waist-to-hip ratio could provide a more comprehensive understanding of obesity’s role in PIH.
As the medical community continues to explore the implications of BMI on surgical outcomes, this study offers valuable insights into optimizing perioperative care for older adults, potentially leading to improved patient safety and reduced healthcare costs.