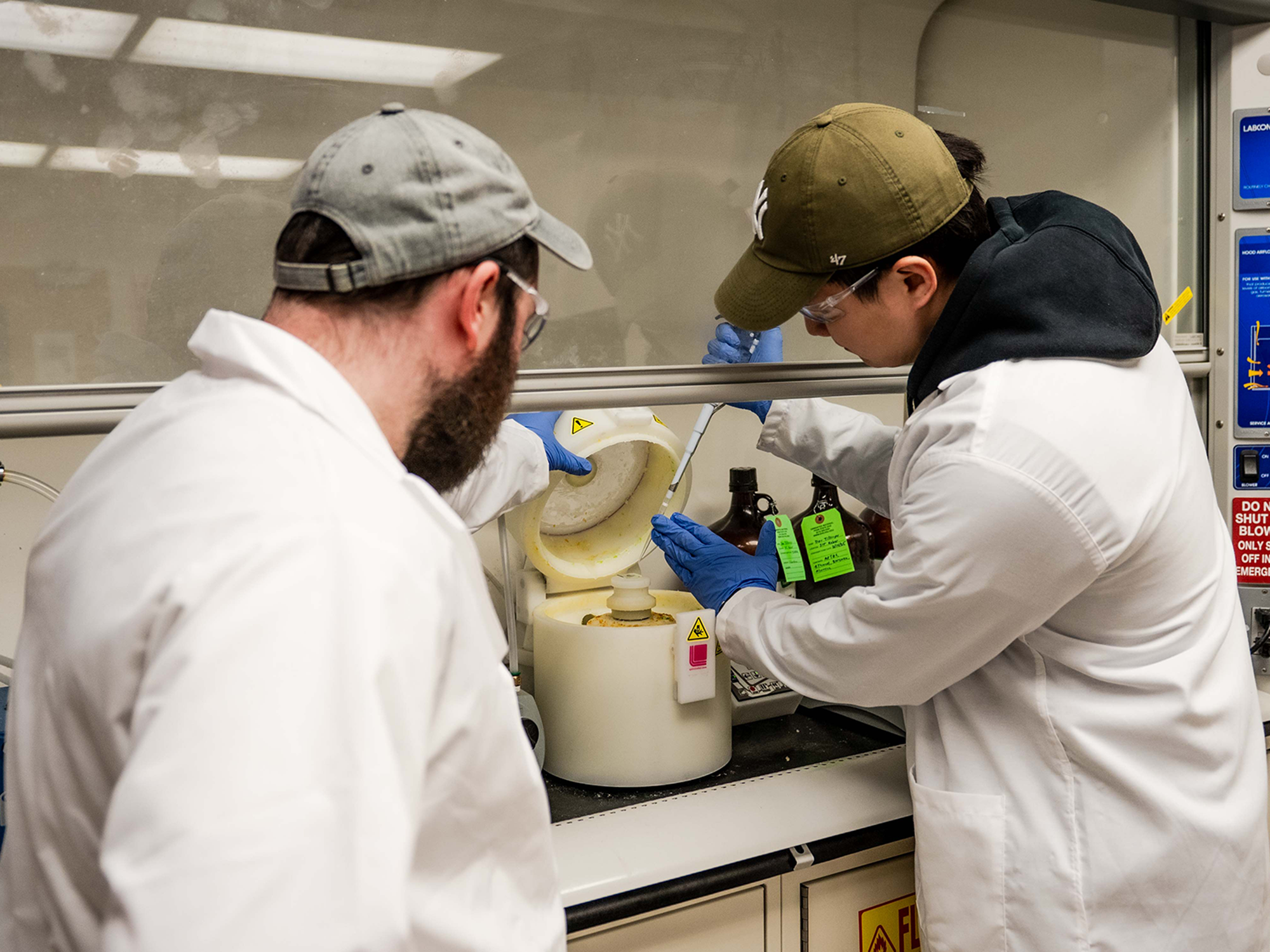
If Wenjun Zhang, a professor of chemical and biomolecular engineering at UC Berkeley, succeeds in her groundbreaking research, the days of brushing and flossing could become a thing of the past. Zhang is on a mission to differentiate the beneficial bacteria in our mouths from the harmful ones responsible for cavities, with the aim of cultivating a probiotic oral microbiome that promotes dental health.
Our mouths host a complex microbiome comprised of hundreds of bacterial species. These bacteria form communities that adhere to teeth, creating plaque. While previous studies have concentrated on identifying species associated with cavities due to their acid production, Zhang’s research delves deeper. Her team is examining the metagenome—the complete set of DNA sequences from all oral bacteria—to pinpoint gene clusters linked to cavities.
Unveiling the Genetic Blueprint
In a recent study published on August 19 in the Proceedings of the National Academy of Sciences, Zhang and her colleagues revealed the discovery of a gene cluster that produces two molecules. These molecules facilitate the formation of a robust biofilm on teeth by helping both beneficial and harmful bacteria adhere together. This gene cluster was identified in certain strains of notorious cavity-causing bacteria, such as Streptococcus mutans.
Zhang envisions a future where this gene cluster could be integrated into beneficial bacteria, enhancing their ability to attach to teeth and outcompete the harmful, acid-producing strains. “After we better understand these molecules’ activity and how they can promote strong biofilm formation, we can introduce them to the good bacteria so that the good bacteria can now form strong biofilms and outcompete all the bad ones,” Zhang explained.
Wenjun Zhang, professor of chemical and biomolecular engineering, UC Berkeley
This research was supported by the National Institute of Dental & Craniofacial Research of the National Institutes of Health (R01DE032732).
Exploring Specialized Metabolism
The gene cluster was identified through an analysis of metagenomic sequences from human volunteers. Berkeley graduate student McKenna Yao conducted a statistical analysis to find clusters associated with oral disease and cultivated the bacteria to study the metabolites they produced. These metabolites, composed of peptides and lipids, enable bacteria to form the sticky biofilm on teeth.
The newly discovered gene cluster contains approximately 15 DNA segments coding for proteins and other elements, forming a “specialized” metabolic cassette. This network, though not essential for bacterial survival, significantly impacts the surrounding environment, such as the teeth. Zhang prefers the term “specialized” over “secondary” metabolism due to the intriguing molecules it can produce.
“These specialized metabolites enhance survival in certain ways,” said McKenna Yao, one of the study’s first authors. “Many, for example, are antibiotics, so they can kill other bugs, or others are involved in metal acquisition—helping bacteria monopolize resources in their niche.”
Despite their potential, the role of specialized metabolic networks in the human microbiome remains largely unexplored. Zhang’s previous research identified a gene cluster in oral bacteria producing an unknown antibiotic, highlighting the importance of these metabolites in human health.
The Future of Oral Health
Understanding the sticky metabolites in the mouth, dubbed mutanoclumpins, could pave the way for new cavity-prevention strategies. “We are looking for something correlated with cavities, with disease. If one day we can prove that, under certain conditions, this is really a bad molecule you want to prevent, we might develop genetic or chemical inhibitors to inhibit their production,” Zhang stated. “Meanwhile, we also look at other molecules correlated with health, allowing a simple strategy to directly engineer the microbes to make more of them.”
One promising candidate for enhancement is Streptococcus salivarius, a bacterium known to promote oral health and currently marketed as an oral probiotic. However, it struggles to form a strong biofilm on teeth. Zhang suggests bolstering its biofilm-forming capabilities to improve its probiotic effectiveness.
“Our future work will be to create a broad map of the collection of these specialized metabolites to look at collectively what this dynamic, complex community on your teeth is making,” Zhang said.
Despite these advancements, Yao cautions that brushing remains the most effective way to remove biofilm. “We believe that there’s actually a better way of disrupting that biofilm, but we’re just beginning to understand what the complexity is within the mouth,” she noted.
The study’s first co-authors include Nicholas Zill and Colin Charles Barber, alongside Yao. Other contributors are Yongle Du, Rui Zhai, Eunice Yoon, and Dunya Al Marzooqi from Berkeley’s Department of Chemical and Biomolecular Engineering, and Peijun Lin, a visiting student in the College of Computing, Data Science, and Society.