Researchers at the Icahn School of Medicine at Mount Sinai, in collaboration with international partners, have announced promising results from a novel mRNA-based therapy aimed at combating antibiotic-resistant bacteria. This groundbreaking study, published in the November 26 issue of Nature Biotechnology, demonstrates that the therapy can effectively slow bacterial growth, enhance immune response, and reduce lung tissue damage in preclinical models of multidrug-resistant pneumonia.
Antibiotic-resistant infections pose a significant global health threat, claiming over 1.2 million lives annually and contributing to nearly 5 million deaths worldwide. In the United States, these infections account for more than 3 million cases each year, resulting in approximately 48,000 deaths and incurring billions in healthcare costs. Experts have raised alarms over the increasing resistance across major bacterial species, jeopardizing routine medical procedures and treatments.
Innovative Approach to a Global Crisis
The novel therapy employs mRNA to instruct the patient’s body to produce a unique infection-fighting protein known as a “peptibody.” This peptibody is engineered to perform dual functions at the site of infection: directly dismantling harmful bacteria and recruiting immune cells to assist in clearing them.
Dr. Xucheng Hou, a lead author of the study and Assistant Professor of Immunology and Immunotherapy at Mount Sinai, explained,
“Our work suggests there may be a new path to tackling antibiotic-resistant infections by supporting the immune system more directly. Although we’re still in the early stages and have only tested this approach in preclinical models, the results lay important groundwork for future therapies that could enhance how traditional antibiotics perform.”
Mechanism of Action
The mRNA is encapsulated in lipid nanoparticles, similar to those used in mRNA vaccines, to ensure safe delivery into the patient’s body. These nanoparticles not only protect the mRNA during transport but also include an additive that mitigates harmful inflammation by neutralizing reactive oxygen species, which are often responsible for tissue damage during infections.
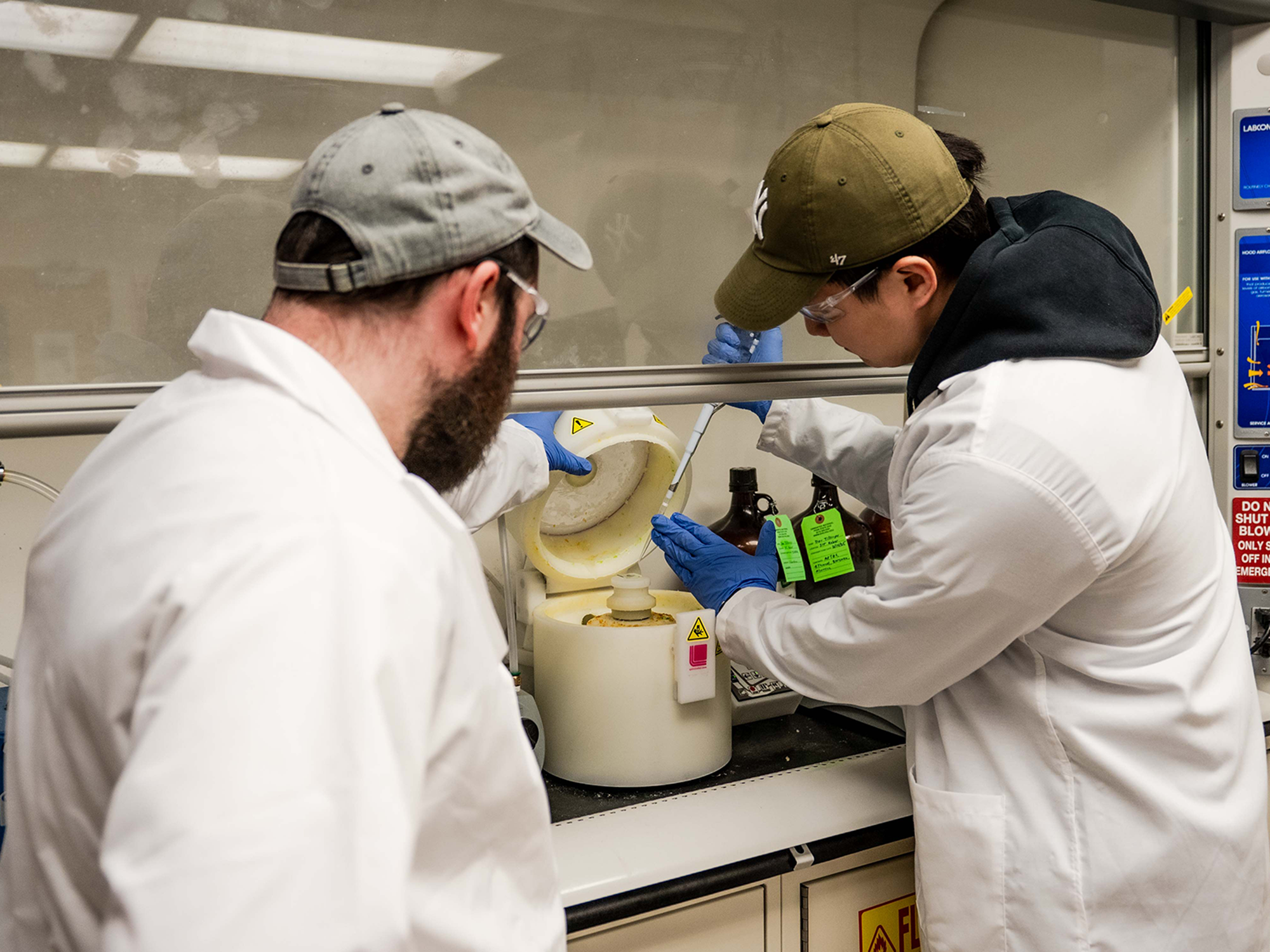
In experiments involving mouse models of multidrug-resistant Staphylococcus aureus and Pseudomonas aeruginosa, the therapy was well tolerated, decreased bacterial presence in the lungs, reduced inflammation, and preserved normal lung architecture. Laboratory tests on human lung tissue mirrored these results, suggesting compatibility with human immune systems.
Future Directions and Implications
The researchers are poised to advance to further preclinical studies, with aspirations to initiate human clinical trials to assess safety, dosing, and efficacy. While still in its nascent stages, this therapy represents a promising new direction in the fight against antibiotic-resistant infections.
Dr. Yizhou Dong, senior author and co-corresponding author of the study, emphasized the potential impact, stating,
“This is the first evidence that an mRNA-encoded antimicrobial peptide can directly kill bacteria while also turning on the immune system’s protective responses. If future studies bear this out, it could open the door to a highly adaptable platform for developing new treatments against infections that no longer respond to today’s antibiotics.”
Broader Context and Support
The study, titled “Antimicrobial peptide delivery to lung as peptibody mRNA in anti-inflammatory lipids treats multidrug-resistant bacterial pneumonia,” was conducted by a team of researchers including Yonger Xue, Xucheng Hou, Siyu Wang, and others. This research received partial funding from the Maximizing Investigators’ Research Award (R35GM144117) from the National Institute of General Medical Sciences.
The announcement comes at a critical time as the medical community grapples with the escalating threat of antibiotic resistance. The potential for mRNA-based therapies to provide a versatile and effective solution marks a significant milestone in medical research, promising to reshape the landscape of infectious disease treatment.
As this innovative approach progresses towards clinical application, it holds the potential to not only enhance current antibiotic efficacy but also to pioneer new strategies in the global battle against resistant infections.