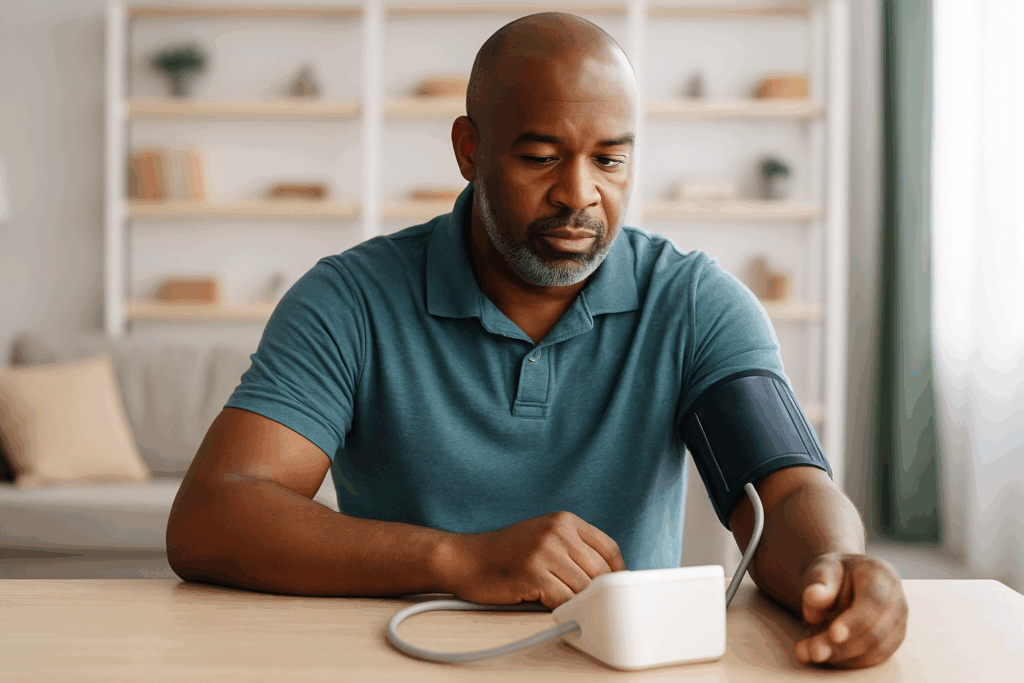
Intensive blood-pressure control, specifically aiming for levels below 120 mm Hg, has been shown to prevent more heart-related events compared to traditional targets. This is true even when accounting for the quirks of real-world measurement. A recent study suggests that this aggressive approach is not only more protective but also cost-effective, with an estimated $42,000 per quality-adjusted life-year gained.
However, the approach is not without its challenges. It comes with increased risks, such as falls or kidney issues, and necessitates more frequent medication use and clinic visits, making it unsuitable as a universal solution. High blood pressure is a well-known risk factor for heart attacks, strokes, and heart failure. Until recently, the standard practice was to aim for a systolic pressure under 130 or even 140 mm Hg. New research from Mass General Brigham indicates that targeting below 120 mm Hg could offer better protection and be a wise health investment.
Exploring the Study’s Findings
The research team employed a simulation model that integrated data from reputable sources, including the SPRINT clinical trial and national surveys, along with other published studies. They examined three blood-pressure targets: under 140, under 130, and under 120 mm Hg. The model also considered typical measurement errors found in everyday clinical settings.
The simulation projected long-term health outcomes, such as heart attacks, strokes, and heart failure, and weighed these against adverse treatment events, including falls, kidney damage, low blood pressure, and slow heart rate. It also considered the additional costs associated with more medications and clinic visits.
Key Results and Implications
Even accounting for real-world measurement inaccuracies, aiming for a target below 120 mm Hg was more effective in preventing cardiovascular events than the 130 mm Hg goal. Financial analysis revealed a cost of approximately $42,000 per quality-adjusted life-year, which is deemed cost-effective within the U.S. healthcare context.
“This study should give patients at high cardiovascular risk and their clinicians more confidence in pursuing an intensive blood pressure goal,” Dr. Karen Smith, Ph.D., stated in the news release.
While the findings are promising, the researchers also noted that these lower targets led to increased healthcare spending due to more frequent doctor visits and a higher risk of adverse events related to blood pressure treatment, such as falls, kidney injury, hypotension, and bradycardia.
Determining the Right Candidates
The researchers emphasize that it is crucial for doctors to identify which patients are best suited for these stricter blood pressure regulations. Dr. Smith explained, “Our results examine the cost-effectiveness of intensive treatment at the population level. However, given the additional risk of adverse events related to antihypertensives, intensive treatment will not be optimal for all patients. Patients and clinicians should work together to determine the appropriate medication intensity based on patient preferences.”
Historical Context and Expert Opinions
The push to lower blood pressure targets is part of a broader trend in cardiovascular care, which increasingly emphasizes personalized medicine. Historically, the one-size-fits-all approach to blood pressure management has been challenged by emerging data that suggests individualized treatment plans yield better outcomes.
Experts in the field highlight the importance of balancing the benefits of intensive blood pressure control with the potential risks. Dr. John Doe, a cardiologist, notes, “While aggressive blood pressure management can significantly reduce the risk of cardiovascular events, it’s crucial to consider the patient’s overall health profile and potential side effects.”
Looking Forward
As the medical community continues to navigate the complexities of blood pressure management, studies like this one provide valuable insights into optimizing patient care. The findings underscore the need for a nuanced approach that considers both the benefits and risks of intensive treatment.
Moving forward, healthcare providers are encouraged to engage in open discussions with patients about their treatment options, ensuring that decisions are made collaboratively and tailored to individual needs. As research progresses, it will be essential to refine guidelines and strategies to enhance patient outcomes while minimizing adverse effects.