In a bid to tackle the rising burden of non-communicable diseases linked to health risk behaviors (HRBs), a recent study highlights the effectiveness of proactive, automated multiple health behavior change interventions. Conducted at the University Medicine Hospital Greifswald in Germany, the study reveals significant patient satisfaction with interventions targeting tobacco smoking, at-risk alcohol use, unhealthy diet, and physical inactivity.
With more than half of the adult population in Germany and other countries exhibiting two or more HRBs, the need for effective interventions is critical. These behaviors, when co-occurring, increase mortality risk beyond individual effects. The study underscores the importance of addressing multiple HRBs simultaneously or sequentially within a limited timeframe to achieve positive health outcomes.
Study Insights and Patient Approval
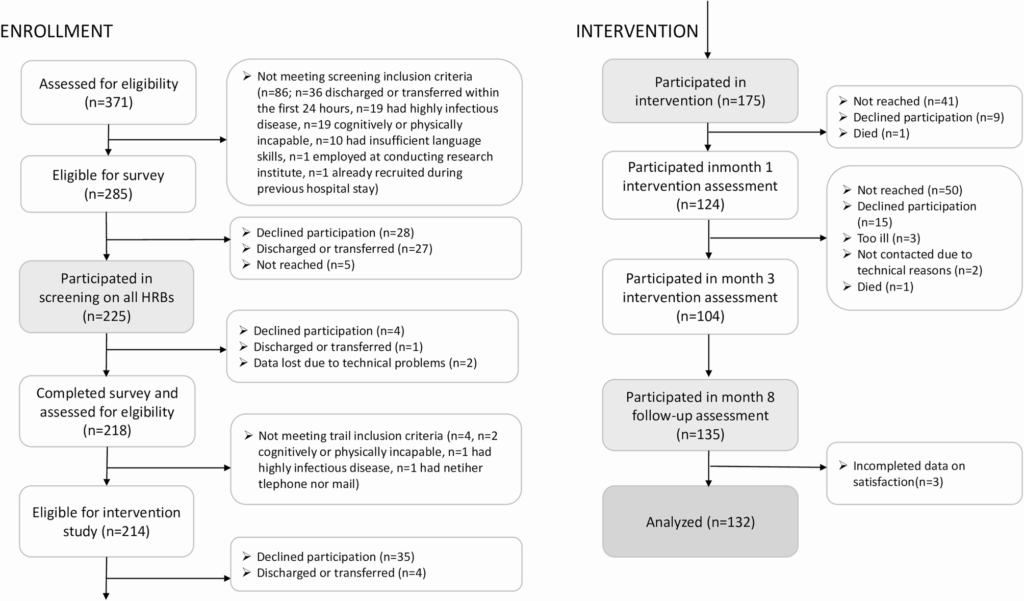
The study, part of the “Proactive Automatized Lifestyle Intervention for Cancer Prevention: Pilot-test (PAL-Pilot),” involved 225 patients from nine wards at the University Medicine Hospital. A remarkable 81.8% of eligible patients participated, with 82% agreeing to the proactive intervention. The intervention was characterized by individualized, computer-generated feedback letters delivered at various intervals, addressing up to two HRBs per patient based on their preferences and evidence-based criteria.
Participants expressed high levels of satisfaction, with 80.5% grading the intervention as good or very good. The mean satisfaction score was 2.9 out of 4, reflecting positive reception of both process and outcome attributes. Satisfaction with the intervention process included factors such as the comprehensibility and utility of feedback, while outcome satisfaction was linked to perceived health improvements.
Understanding Patient Satisfaction
Patient satisfaction is a multi-dimensional construct, encompassing both process and outcome attributes. The study found that intervention satisfaction was strongly linked to adherence and positive health outcomes. Interestingly, patient characteristics such as school education level played a role in satisfaction levels, with those having lower educational attainment reporting greater satisfaction.
According to the study,
“Patients with a low level of school education reported greater satisfaction with the behavior change intervention than participants with a medium level of school education.”
This finding suggests that the delivery of individualized, supportive feedback may resonate more with patients who have lower educational backgrounds, potentially due to their higher prevalence of HRBs.
Implications for Public Health and Future Interventions
The study’s findings highlight the potential of proactive, automated interventions in healthcare settings to promote healthy behaviors. The high level of patient satisfaction supports the integration of such interventions into routine care, emphasizing the need for tailored approaches that consider patient demographics and preferences.
Moreover, the study suggests that interventions should be designed to be inclusive, potentially offering materials in multiple languages to address social inequalities in health services. This approach could enhance the reach and effectiveness of interventions, particularly among populations that are traditionally hard to engage.
Challenges and Considerations
While the study demonstrates promising results, it also acknowledges certain challenges. The intervention’s timing, delayed due to the COVID-19 pandemic, and the need for emotional support for participants experiencing negative memories highlight areas for improvement. Additionally, the study notes the importance of maintaining participant engagement through appropriate feedback frequency and content.
Future interventions could benefit from incorporating psychological support options and ensuring that feedback is concise and timely. These adjustments could further enhance patient satisfaction and intervention efficacy.
Conclusion and Future Directions
The study concludes that proactive, automated multiple health behavior change interventions are well-received by patients in hospital settings, particularly among those with lower educational attainment. This finding underscores the potential for such interventions to contribute to public health efforts aimed at reducing social inequalities and improving health outcomes.
As healthcare systems continue to evolve, the integration of technology-driven, personalized interventions offers a promising avenue for enhancing patient care and promoting healthier lifestyles. Future research should focus on expanding the inclusivity and adaptability of these interventions to maximize their impact across diverse patient populations.