Millions of Americans seek urgent treatment for urinary tract infections (UTIs) each year, a condition that is both painful and often embarrassing. Traditionally, this required an in-person visit for testing and treatment. However, the landscape of UTI care has shifted dramatically with the advent of telehealth and direct-to-consumer healthcare options, allowing patients to consult with healthcare providers via phone or video, and even purchase rapid UTI tests at local drugstores.
While these innovations offer convenience and speed, they also pose significant risks, including the overuse of antibiotics and underuse of urine culture tests. This is particularly concerning for women who frequently experience UTIs. The over-prescription of antibiotics contributes to the rise of antibiotic-resistant bacteria, commonly known as “superbugs.”
Introducing the Ann Arbor Guide
A new guide published in the JAMA Network Open by a team from the VA Ann Arbor Healthcare System and the University of Michigan Medical School seeks to address these challenges. The Ann Arbor Guide to Triaging Adults with Suspected UTI is designed for the modern age of telehealth and aims to help clinicians make informed decisions about testing and prescribing antibiotics for patients with UTI-like symptoms.
The guide was developed as part of a patient safety project funded by the VA National Center for Patient Safety. It includes two algorithms—one for non-pregnant women and another for men—that provide clear instructions on when to order tests and prescribe antibiotics. These algorithms are presented in colorful, easy-to-follow formats in the guide’s supplement.
Addressing a Growing Concern
Dr. Jennifer Meddings, the first author of the paper and a primary care clinician at the VAAAHS and Michigan Medicine, highlights the evolving nature of UTI care. “Clinics have long had triage systems for uncomplicated UTIs, especially for healthy women,” she explains. “However, virtual care and online services that deliver prescriptions based on questionnaires have changed the landscape significantly.”
Dr. Meddings notes that UTIs are one of the most common reasons for antibiotic prescriptions in the U.S., and the rise of resistant bacteria is a growing concern. The shortage of primary care providers and appointments has exacerbated the situation, leading to fewer in-person visits where urine samples can be collected and cultured.
“It’s more important than ever for providers to know which patients can safely receive antibiotics empirically,” Dr. Meddings emphasizes, “without relying solely on dipstick tests or no tests at all.”
Guidance for Complex Scenarios
The Ann Arbor UTI Guide was developed using the RAND/UCLA Appropriateness Method, which synthesizes expert opinion. It addresses not only straightforward cases but also complex scenarios involving patients with conditions like organ transplants, chemotherapy, immunosuppression, kidney disease, and recurrent UTIs.
The guide includes triage instructions for symptoms that might indicate more serious conditions, such as sexually transmitted infections, kidney infections, or sepsis. Karen Fowler, a patient safety specialist at the VA Center for Clinical Management Research, notes that the guide is being piloted for use in telehealth visits for Veterans at local VA health centers.
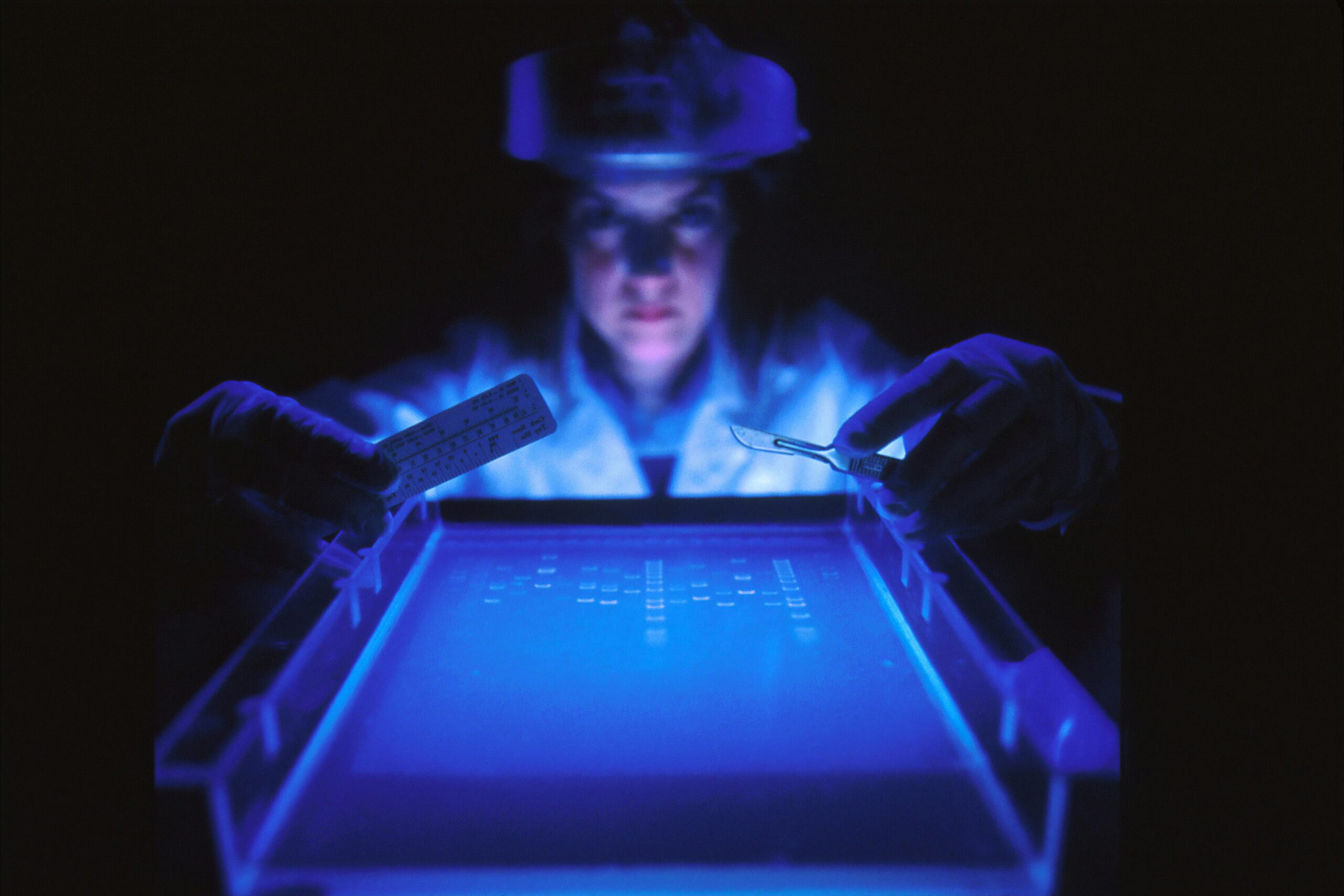
Emphasizing Accurate Testing
While at-home UTI tests are convenient, the guide’s authors caution that they are not sufficiently accurate to confirm a UTI. They recommend confirming UTI diagnoses with urine cultures, especially in cases where clinical urinalysis results are abnormal.
U-M Health has adopted a “urinalysis with reflex to culture” strategy, meaning that most patients with negative rapid urine tests won’t have their urine cultured, but those with positive results will. This approach aims to balance the need for accurate diagnosis with the practicalities of telehealth.
“We hope this guide will help both patients and providers recognize that virtual consultations alone may not suffice for accurate diagnosis or treatment,” Dr. Meddings asserts. “However, telehealth has removed barriers to care, such as transportation and time off work.”
The guide’s authors include a team of experts from U-M and VA, who emphasize the importance of requesting urine cultures, especially for women who frequently experience UTIs and most men, even when using virtual services.
As telehealth continues to evolve, the Ann Arbor Guide represents a critical step in ensuring that UTI care remains both effective and safe, balancing the benefits of modern healthcare innovations with the necessity of antibiotic stewardship.