Researchers at Northern Arizona University (NAU) are pioneering a novel approach that could enable clinicians to identify Alzheimer’s disease at an earlier stage and potentially slow its progression. This innovative project, spearheaded by Travis Gibbons, an assistant professor in the Department of Biological Sciences, focuses on the critical role of brain metabolism in Alzheimer’s development.
Supported by a grant from the Arizona Alzheimer’s Association, Gibbons and his team are investigating how the brain utilizes glucose—the essential sugar that fuels cognitive functions, movement, and emotions. “The brain is like a muscle,” Gibbons explained.
“It needs fuel to do work, and its gasoline is blood glucose. A healthy brain is greedy; it burns through glucose fast. But brain metabolism is slower when you have Alzheimer’s. It can be viewed as a canary in the coal mine in the development of the disease.”
Tracking Brain Glucose Metabolism Without Invasive Procedures
Historically, measuring glucose metabolism in the brain has posed significant challenges due to its inaccessibility. Previous studies involved invasive techniques, such as inserting catheters into neck veins to collect blood samples leaving the brain—methods unsuitable for routine checkups.
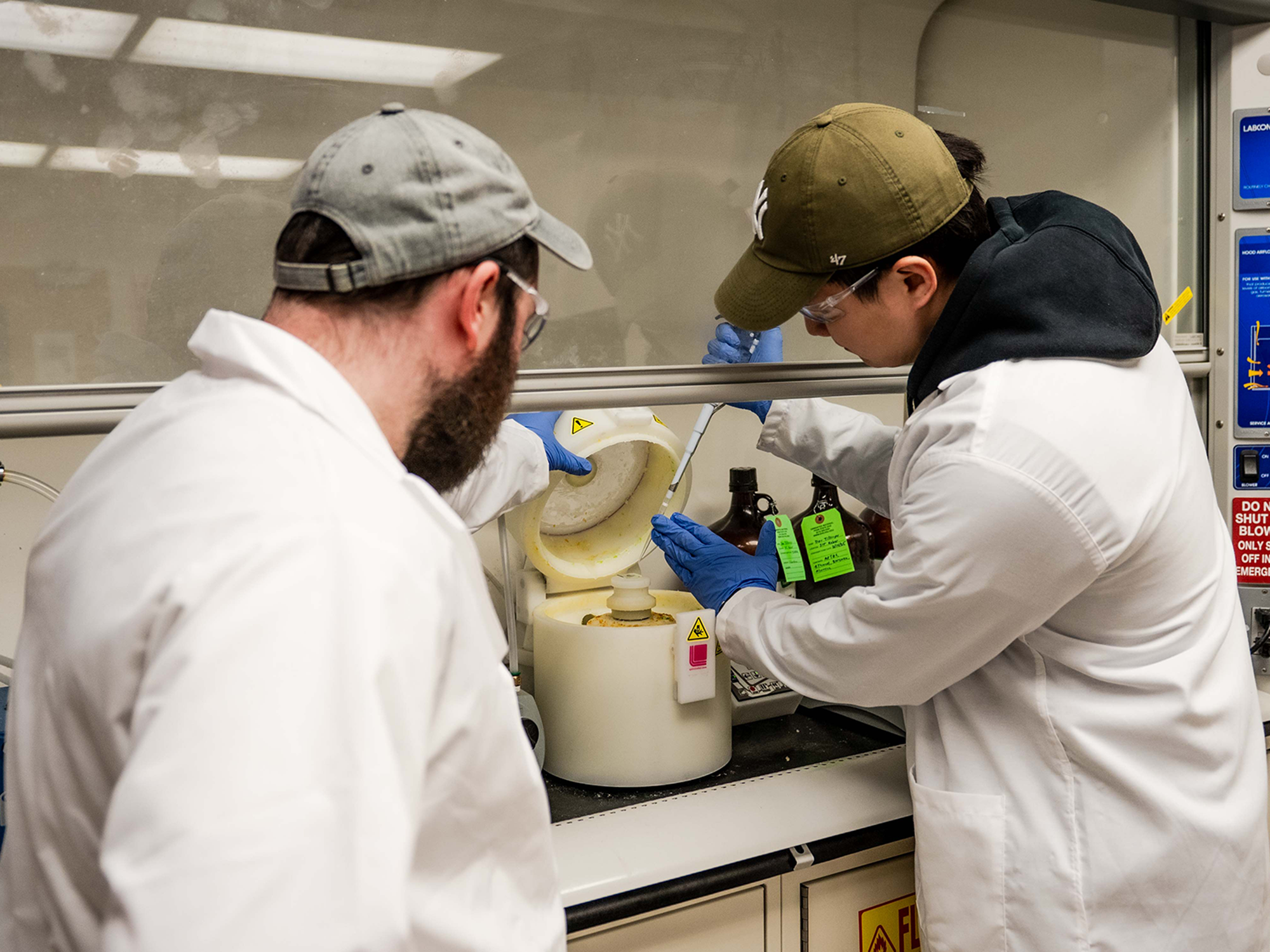
However, Gibbons and his team are now exploring a less invasive alternative using commercially available kits designed to isolate and analyze microvesicles circulating in the bloodstream. “Some of these microvesicles originate in a neuron in your brain, and they’re like messengers carrying cargo,” Gibbons noted.
“With these test kits, we can find what kind of cargo is in a microvesicle and run tests on it. It’s been described as a biopsy for the brain, but much less invasive. That’s the appeal of it.”
Microvesicles as a Potential “Biopsy for the Brain”
The development of this method could revolutionize how Alzheimer’s is detected and monitored over time. Although the process is still under refinement, its potential impact is substantial. Gibbons emphasized that while the workflow is demanding and requires meticulous technique, the possible benefits are significant.
In a previous study, Gibbons and his colleagues administered insulin nasally, a method that enhances its delivery to the brain compared to traditional injections. Following this, the team collected blood leaving the brain and identified biomarkers associated with improved neuroplasticity. They are now striving to detect these biomarkers within microvesicles.
Study Stages From Healthy Volunteers to Alzheimer’s Patients
The research is advancing methodically. Initially, Gibbons is validating the approach with healthy participants. The next phase involves comparing results among individuals with mild cognitive impairment and those diagnosed with Alzheimer’s to determine if shifts in glucose metabolism can effectively track disease progression.
“Brain function is notoriously hard to measure, but we’re getting better and better at interrogating brain function through biomarkers,” Gibbons remarked.
“Soon, we might be able to help people protect their brain health and prevent Alzheimer’s disease the same way we protect people from cardiovascular disease by prescribing moderate exercise and a healthy diet. That will help us manage the burden on aging people and society as a whole.”
Gibbons, a member of the Arizona Alzheimer’s Consortium (AAC), is conducting the study alongside Emily Cope, an NAU associate professor of biological sciences and fellow AAC member; K. Riley Connor, a Ph.D. student in biological sciences at NAU; and Philip Ainslie, a professor at the University of British Columbia’s Centre for Heart, Lung & Vascular Health.
The announcement comes as the global medical community intensifies efforts to combat Alzheimer’s, a disease that affects millions worldwide. The move represents a significant step forward in the ongoing quest to understand and mitigate the impact of neurodegenerative diseases.
As the research progresses, the team hopes to pave the way for new diagnostic tools that could transform Alzheimer’s care. The implications of this work extend beyond individual patients, offering potential societal benefits by reducing the overall burden of Alzheimer’s and improving quality of life for aging populations.