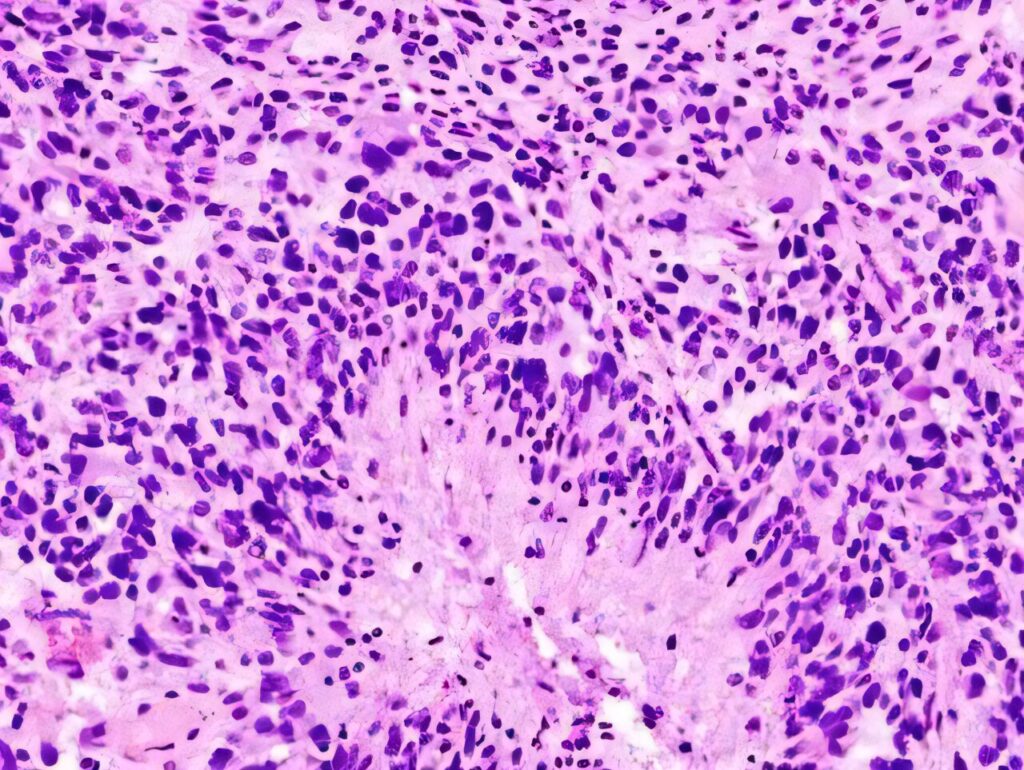
A groundbreaking study from the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine has uncovered a surprising mechanism in glioblastoma cells that could explain their deadly nature. Researchers found that glioblastoma cells that disperse from clusters become more aggressive and deadly compared to those that remain clustered. This discovery, also observed in breast cancer samples, suggests a potential new principle in solid tumor biology.
The study, led by Dr. Anna Lasorella and Dr. Antonio Iavarone, was published in the journal Cancer Cell. “This gives us a much better grasp of the biology of glioblastoma, a tumor type where a lot still remains to be discovered,” said Lasorella, the senior author of the paper.
Understanding Glioblastoma’s Aggressiveness
Glioblastoma is notoriously difficult to treat, with patients typically surviving only slightly more than a year post-diagnosis. The cancer often recurs after initial treatment, with recurring tumors showing resistance to therapy. The study provides a potential explanation for this resilience: dispersed glioblastoma cells exhibit greater plasticity, meaning they can change forms or states more easily, a trait linked to treatment resistance and poorer patient outcomes.
“There has never really been an integrated explanation as to why cancer cells develop plasticity,” said Iavarone. “That’s what our study does. We’ve now revealed how the plasticity of glioblastoma cells is controlled.”
Initial treatments like chemotherapy or radiation might inadvertently break up less harmful clusters of cancer cells, causing them to disperse and become more plastic. This hypothesis, while yet to be tested, highlights the complex behavior of clustered versus dispersed cells within tumors.
Technological Advances in Cancer Research
The research utilized the CosMx platform, a cutting-edge technology that allows scientists to profile thousands of genes in individual cells within a tumor. This spatial transcriptomics approach provides detailed insights into the types of cells present and their locations relative to each other.
In previous studies, the researchers identified four types of glioblastoma cells based on gene expression. This study further examined how these cell types are organized within tumors, finding both clusters of similar cells and mixed, dispersed areas. The dispersed cells were found to be more plastic, lacking the proteins that help clustered cells stick together.
Implications for Other Cancers
The principles observed in glioblastoma were also evident in breast cancer samples, suggesting a broader relevance for solid tumors. Dispersed cancer cells in breast cancer were similarly more plastic than those in clusters, indicating a potential universal mechanism driving tumor metastasis.
“We think this principle is of general significance for solid tumors,” said Iavarone. “It provides an answer to why certain cells become so aggressive.”
Future Directions and Potential Treatments
The researchers are now exploring whether promoting cell clustering could prevent the dispersal and increased plasticity of tumor cells. They have demonstrated that disrupting cell adhesion leads to more dispersed cells in pre-clinical glioblastoma models, though reversing this process presents a challenge.
Another avenue of investigation involves identifying proteins or molecules that dispersed cells might express to disrupt adhesion. Targeting these proteins could offer new drug development opportunities.
“If we can better understand this mechanism, we hope to one day be able to maintain the clustered cells that are less plastic in that state, or even reverse the dispersal of these more plastic cells,” said Lasorella.
As research progresses, these findings could pave the way for innovative treatments that tackle the core mechanisms of tumor aggressiveness, potentially improving outcomes for patients with glioblastoma and other solid tumors.