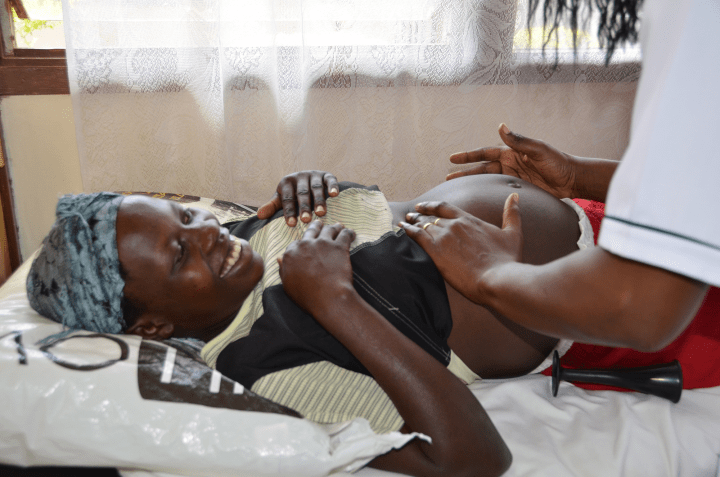
Women who lose 300ml of blood after giving birth should now be diagnosed with postpartum haemorrhage (PPH), according to new guidelines published by the World Health Organization (WHO), the International Federation of Gynaecology and Obstetrics (FIGO), and the International Confederation of Midwives (ICM). Previously, PPH was diagnosed only when a woman lost 500ml of blood, a threshold that often delayed timely intervention.
The announcement comes as a significant shift in maternal health protocols, urging doctors and midwives to closely monitor women post-birth using a calibrated drape, a device that accurately measures blood loss. Once PPH is diagnosed, the guidelines recommend the immediate use of the MOTIVE bundle: Massage of the uterus, Oxytocic drugs, Tranexamic acid (TXA), Intravenous fluids, Vaginal and genital tract examination, and Escalation of care if necessary.
Impact of Postpartum Haemorrhage
PPH affects millions of women globally each year and remains one of the leading causes of maternal mortality, responsible for nearly 45,000 deaths annually. Beyond fatalities, PPH can lead to severe long-term health issues, including major organ damage, hysterectomies, and mental health challenges such as anxiety and trauma.
“Postpartum haemorrhage is the most dangerous childbirth complication since it can escalate with such alarming speed. While it is not always predictable, deaths are preventable with the right care,” said Dr. Jeremy Farrar, WHO Assistant Director-General.
According to Dr. Farrar, the new guidelines aim to maximize impact where the burden is highest and resources are most limited, ensuring more women survive childbirth and return home safely.
Research and Recommendations
The motivation for this change stems from a large study published in The Lancet, which analyzed data from 312,151 women. The study found that a blood loss of 300ml provided the “preferred sensitivity threshold,” especially when accompanied by abnormal haemodynamic signs like increased pulse rate or decreased blood pressure.
In cases where bleeding persists, the guidelines also advise surgical intervention or blood transfusions to stabilize the patient. FIGO President Professor Anne-Beatrice Kihara emphasized the need for care that is “fast, feasible, effective” to drive progress toward eliminating PPH-related deaths.
“These guidelines take a proactive approach of readiness, recognition, and response. They are designed to ensure real-world impact – empowering health workers to deliver the right care, at the right time, and in a wide range of contexts,” said Professor Kihara.
Preventive Measures and Broader Implications
The guidelines also highlight the importance of good antenatal and postnatal care to mitigate risk factors such as anaemia, which increases the likelihood of PPH. Recommendations include daily oral iron and folate during pregnancy and intravenous iron transfusions when rapid correction is needed.
Additionally, the guidance discourages routine episiotomies to reduce trauma and severe bleeding. During the third stage of labor, administering medicine to support uterine contraction, such as oxytocin or carbetocin, is recommended. Misoprostol may be used as a last resort if intravenous options are unavailable.
Call to Action
Professor Jacqueline Dunkley-Bent, ICM’s Chief Midwife, stressed the urgency of adopting these guidelines. “Midwives know first-hand how quickly postpartum haemorrhage can escalate and cost lives. These guidelines are a game-changer. But to end preventable deaths from PPH, we need more than evidence and protocols. We call on governments, health systems, donors, and partners to step up, adopt these recommendations quickly, and invest in midwives and maternal care.”
According to a commentary in The Lancet, the new guidelines are “an equity intervention” that aligns the prevention-detection-treatment continuum with supportive infrastructure, reducing ambiguity in emergency situations.
The move represents a critical step forward in maternal health, aiming to combat the infodemic in health information and support health policy reporting from the global South. As these guidelines are implemented, they hold the promise of transforming maternal care and reducing preventable deaths worldwide.