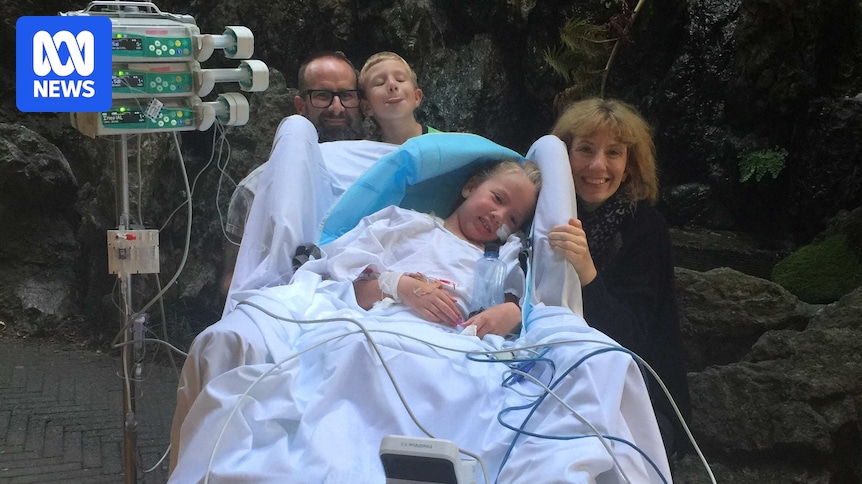
After skipping her flu vaccine for just one year, Millie Campbell found herself in a life-threatening battle. In 2019, the then-eight-year-old contracted influenza B, which began with leg aches and escalated to multiple organ failure.
“They had to drain 200 millilitres of fluid from her heart — it was struggling,” recalled her mother, Stephanie Campbell. “I think the doctor’s words were ‘your daughter could die tonight’.”
Millie’s parents were faced with the terrifying possibility of losing their daughter. She was airlifted from Newcastle to Westmead Children’s Hospital in Sydney, where she soon went into cardiac arrest. “It was very, very surreal, it actually felt like at the time it wasn’t happening,” said her father, Ian Campbell.
Influenza B’s Impact on Children
This year, Australia has witnessed a significant rise in influenza B cases, particularly among children aged five to 16, despite influenza A being the more common virus type. Influenza B can be more severe in children, although both types present similarly. The standard influenza vaccine includes two strains each of the A and B viruses.
According to Patrick Reading, director of the World Health Organization Collaborating Centre for Reference and Research on Influenza, “Influenza B often gets a reduced awareness compared to influenza A, probably because A is normally associated with pandemics.”
Children currently make up the highest proportion of influenza B cases in Australian hospitals, though the reason remains unclear.
“It’s a bit of a mystery. It’s an association that we see, but we can’t say there’s something specific about the virus that means it infects more children over adults,” Professor Reading explained.
Declining Vaccination Rates and Public Confusion
Flu vaccination rates have been declining since the COVID-19 pandemic, with the most affected group — children aged five to 16 — showing the lowest vaccination uptake. “In 2022, we had high rates across all age groups, and now we have so many unvaccinated people, which means we have a larger cohort of people who are susceptible to infection,” noted Professor Reading.
Julie Leask, a social scientist specializing in vaccination, highlighted the confusion surrounding vaccine recommendations. “I don’t think the risk-based strategy is working well for Australia,” she said. “When the vaccine is on the [National Immunisation Program], it’s a real signal to people that this vaccine is important.”
Research indicates that common reasons for not vaccinating children include lack of awareness, healthcare provider recommendations, and affordability.
The current system offers free influenza vaccines under the National Immunisation Program for children between six months and five years old, and again for those 65 and over. However, the cost for others, around $25, may deter some parents.
The Role of Misinformation
The spread of misinformation, particularly from figures like US health secretary and anti-vaccine activist Robert F. Kennedy Jr., has compounded the issue. His recirculation of debunked myths about vaccines has influenced public perception, including in Australia.
“We are seeing from the US this kind of mainstreaming of misinformation,” Professor Leask commented. “We will see the impacts of that to some degree in Australia.”
Millie’s Journey and a Call to Action
Despite her ordeal, Millie Campbell’s story has a positive turn. Now 14, she has become a competitive swimmer, winning multiple gold medals at national championships and setting her sights on the 2028 Paralympics in Los Angeles.
Her parents, however, remain concerned about the shifting attitudes toward vaccination. “This growing hesitancy seems to be driven by the inability of people to decipher between evidence-based information and misinformation on social media,” Mr. Campbell said.
He urged, “Vaccination benefits not only you but the community.” As Australia continues to grapple with influenza B, the Campbells’ message underscores the importance of informed health decisions and community protection.