Implementation science is increasingly recognized as a crucial element in the translation of clinical practice guidelines into everyday healthcare settings. This emerging field focuses on understanding and promoting the systematic uptake of research findings and evidence-based practices into routine practice, thereby improving the quality and effectiveness of healthcare services.
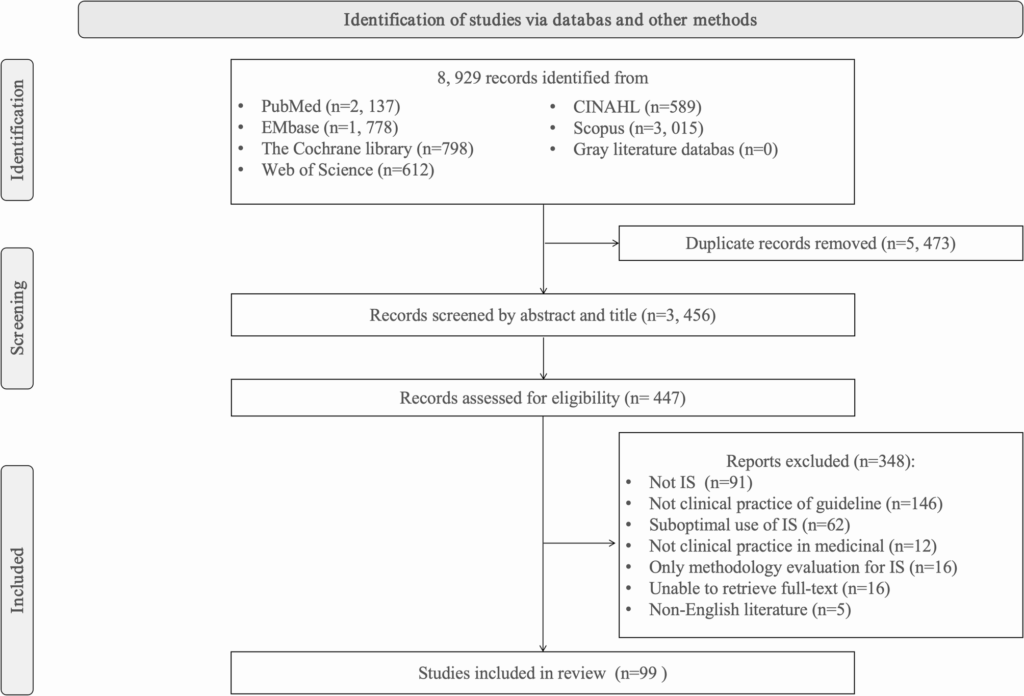
The significance of implementation science has been underscored by numerous studies and reviews, including a comprehensive scoping review conducted by Peters et al. in 2022. This review highlighted the trends in guideline implementation and the challenges faced by healthcare providers in adopting these guidelines effectively. The review emphasized that while guidelines are developed to improve patient outcomes, their actual implementation often lags, leading to a gap between evidence and practice.
The Importance of Clinical Practice Guidelines
Clinical practice guidelines are systematically developed statements that assist practitioners and patients in making decisions about appropriate healthcare for specific clinical circumstances. The Institute of Medicine, in its 2011 report “Clinical Practice Guidelines We Can Trust,” laid out standards for developing trustworthy guidelines, emphasizing their role in enhancing patient care.
Despite their potential, the adoption of clinical guidelines in practice is not always straightforward. Pronovost, in a 2013 JAMA article, highlighted the barriers physicians face, such as lack of awareness, familiarity, and agreement with the guidelines. These barriers can significantly hinder the effective implementation of guidelines in clinical settings.
Implementation Science: A Critical Component
Implementation science seeks to address these challenges by providing a framework for understanding the factors that influence the adoption, implementation, and sustainability of evidence-based interventions. Bauer and Kirchner, in their 2020 article, defined implementation science as a field that “aims to improve the uptake and integration of research findings into healthcare policy and practice.”
One of the key contributions of implementation science is the development of theories, models, and frameworks that guide the implementation process. For instance, the Consolidated Framework for Implementation Research (CFIR) provides a comprehensive structure for identifying factors that influence implementation outcomes, as demonstrated in numerous studies, including those by Thoonsen et al. in 2024.
Challenges in Implementation
The process of implementing clinical guidelines is fraught with challenges. According to a study by Morris et al. in 2011, it takes an average of 17 years for research evidence to reach clinical practice. This delay can be attributed to various factors, including organizational barriers, lack of resources, and resistance to change among healthcare professionals.
Furthermore, the complexity of healthcare systems can impede the implementation process. Chan et al. in 2022 argued that implementation science is a “critical but undervalued part of the healthcare innovation ecosystem,” highlighting the need for a more integrated approach to overcome these systemic challenges.
Moving Forward: Strategies for Success
To enhance the implementation of clinical practice guidelines, several strategies have been proposed. These include the development of tailored interventions that consider the specific context and needs of healthcare providers and patients. For example, the Exploration, Preparation, Implementation, Sustainment (EPIS) framework, reviewed by Moullin et al. in 2019, offers a structured approach to guide the implementation process across different stages.
Moreover, engaging stakeholders, including healthcare providers, patients, and policymakers, is crucial for successful implementation. Proctor et al. in 2012 emphasized the importance of collaboration and communication among all parties involved to ensure that guidelines are not only adopted but also adapted to fit the local context.
“The role as a champion is to not only monitor but to speak out and to educate,” noted Goedken et al. in their 2019 study, underscoring the importance of leadership and advocacy in driving guideline implementation.
Conclusion: The Future of Implementation Science
As healthcare continues to evolve, the role of implementation science in bridging the gap between research and practice becomes increasingly vital. By addressing the barriers to guideline adoption and fostering a culture of continuous improvement, implementation science can help ensure that patients receive the highest standard of care based on the best available evidence.
Moving forward, it is essential for healthcare organizations to invest in implementation science research and training, thereby equipping healthcare professionals with the tools and knowledge needed to navigate the complexities of guideline implementation. As the field continues to grow, it holds the promise of transforming healthcare delivery and improving patient outcomes worldwide.