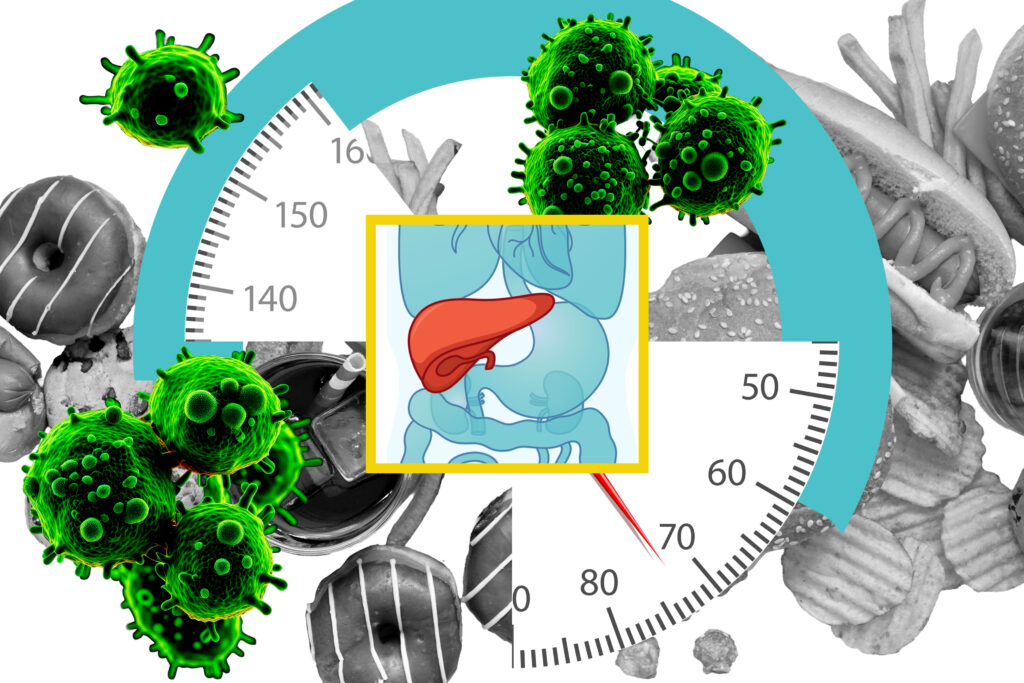
In a groundbreaking study, researchers from the Massachusetts Institute of Technology (MIT) have uncovered a significant link between high-fat diets and an increased risk of liver cancer. The study, published in the journal Cell, reveals how a fatty diet can rewire liver cells, making them more susceptible to becoming cancerous.
The research team, led by Alex K. Shalek, director of the Institute for Medical Engineering and Sciences at MIT, found that a high-fat diet prompts mature liver cells, known as hepatocytes, to revert to an immature, stem-cell-like state. This cellular shift, while initially a survival mechanism against the stress of a fatty diet, ultimately increases the likelihood of cancer development.
Understanding the Cellular Reversion
According to the study, the reversion of hepatocytes is controlled by several transcription factors, which could serve as potential drug targets to prevent tumor development in high-risk individuals. Shalek, along with Ömer Yilmaz and Wolfram Goessling, are senior authors of the study, which also involved contributions from MIT graduate student Constantine Tzouanas and other researchers.
The study explored the effects of a high-fat diet on liver cells by feeding mice such a diet and conducting single-cell RNA-sequencing at various stages of liver disease progression. This approach allowed the team to monitor gene expression changes as the mice moved from liver inflammation to tissue scarring and eventually cancer.
“If cells are forced to deal with a stressor, such as a high-fat diet, over and over again, they will do things that will help them survive, but at the risk of increased susceptibility to tumorigenesis,” Shalek explains.
Implications for Human Health
The findings from the mouse model were further corroborated by analyzing human liver tissue samples. The researchers discovered that similar gene expression patterns were present in patients with liver disease, indicating a decreased expression of genes necessary for normal liver function and an increase in genes associated with immature cellular states.
This discovery is significant as it provides a potential predictive tool for patient outcomes. Patients exhibiting higher expression of pro-survival genes linked to high-fat diets had shorter survival times after tumor development. Conversely, lower expression of genes supporting normal liver functions also correlated with reduced survival.
“Patients who had higher expression of these pro-cell-survival genes that are turned on with high-fat diet survived for less time after tumors developed,” Tzouanas notes.
Future Directions and Research
The researchers are now focused on determining whether the cellular changes induced by a high-fat diet can be reversed. They aim to explore the effects of returning to a normal diet or using weight-loss drugs like GLP-1 agonists. Additionally, the team is investigating whether the identified transcription factors could be viable drug targets to prevent the progression of liver disease to cancer.
While the study in mice showed cancer development within a year, the researchers estimate that in humans, this process could take up to 20 years, influenced by individual risk factors such as diet, alcohol consumption, and viral infections.
The study was supported by funding from the Fannie and John Hertz Foundation Fellowship, the National Science Foundation Graduate Research Fellowship, the National Institutes of Health, and the MIT Stem Cell Initiative through Foundation MIT.
This research not only highlights the potential dangers of high-fat diets but also opens new avenues for therapeutic intervention, offering hope for improved outcomes for patients at risk of liver cancer.