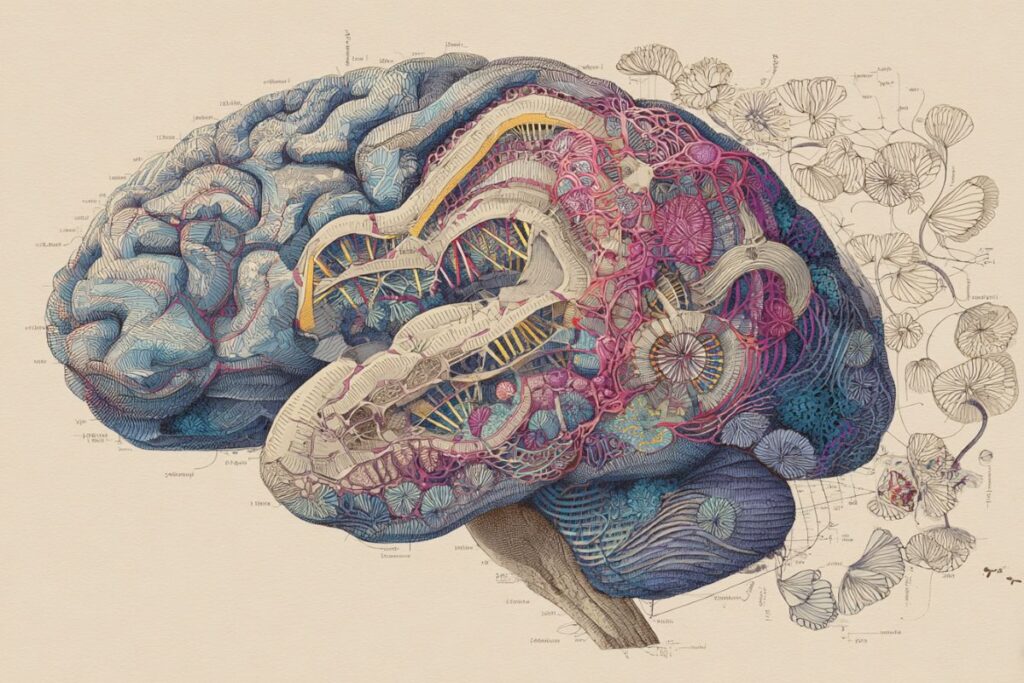
New research has unveiled that depression manifesting before the age of 25 has a significantly stronger hereditary component compared to cases that emerge later in life. This groundbreaking study analyzed genetic data from over 150,000 individuals diagnosed with depression, identifying distinct genetic regions specifically linked to early-onset cases. Individuals with a high genetic risk for early-onset depression were found to be twice as likely to attempt suicide within a decade, emphasizing the need for early intervention strategies.
The study, conducted by researchers at Karolinska Institutet and published in Nature Genetics, highlights a critical window for intervention that could potentially guide personalized suicide-prevention strategies. The findings underscore the importance of genetic information in identifying individuals at high risk of suicide, thereby enabling healthcare professionals to provide more targeted support and closer monitoring.
Early-Onset Depression: A Strong Genetic Influence
Depression is a prevalent mental illness affecting individuals at various stages of life. However, the new study reveals that depression beginning before age 25 exhibits a stronger genetic influence than depression that starts later. The research, which involved medical records and genetic data from over 150,000 people with depression and 360,000 controls across Denmark, Sweden, Norway, Finland, and Estonia, compared the genetics and suicide risk of individuals with early-onset depression to those diagnosed after age 50.
The genetic differences between these groups were substantial. Researchers identified twelve genetic regions linked to early-onset depression, compared to just two regions associated with late-onset cases. This discovery points to the distinct genetic architectures underlying these two forms of depression.
Key Findings: One in four individuals with a high genetic risk of early-onset depression attempted suicide within ten years of diagnosis, a rate nearly double that of those with a lower genetic risk.
Implications for Precision Medicine in Psychiatry
According to Lu Yi, a senior researcher at the Department of Medical Epidemiology and Biostatistics at Karolinska Institutet, the study represents a significant step towards precision medicine in psychiatry. “We show that early-onset depression has partly different genetic causes than depression affecting older individuals and that the risk of suicide attempts is increased,” Yi stated. This insight could lead to more personalized treatment and preventive measures tailored to individual genetic profiles.
The researchers are now planning to explore how these genetic differences relate to brain development, stress, and life experiences. They aim to determine whether genetic risk profiles can be effectively used in suicide prevention strategies within healthcare settings.
Collaborative Efforts and Future Directions
The study is a collaborative effort involving institutions such as the University of Oslo, Copenhagen University Hospital, Roskilde University, and the University of Tartu, alongside the Nordic research network TRYGGVE. It has received funding from the European Research Council (ERC) and the US National Institute of Mental Health, among others.
While some authors have collaborations with pharmaceutical companies, these are unrelated to the current study, ensuring the integrity of the research findings. The study’s results open new avenues for understanding the genetic underpinnings of depression and developing targeted interventions.
By the Numbers: The absolute risk for suicide attempt was 26% in individuals in the top polygenic risk score (PRS) decile for early-onset depression, compared to 12% in the bottom decile and 20% in the intermediate group.
As the research progresses, it holds the promise of informing precision psychiatry approaches for major depressive disorder (MDD), offering hope for more effective and individualized treatment strategies. The findings suggest that early-onset and late-onset depression have partially distinct genetic signatures, with specific developmental brain signatures for early-onset cases.
The study’s insights into the genetic roots of depression and associated suicide risks underscore the potential for genetics to guide future mental health interventions, ultimately aiming to reduce the burden of depression and improve outcomes for those at risk.