Terminally ill patients in Victoria are increasingly finding themselves trapped in hospital palliative care units due to delays in National Disability Insurance Scheme (NDIS) applications. This situation, known as “bed block,” is causing significant distress for both patients and healthcare providers, as reported by palliative care specialists and advocates.
The delays mean that younger patients, who could be receiving care at home or in more suitable accommodations, remain in hospital beds for extended periods. This not only affects their quality of life but also limits access for other terminally ill patients who need these beds. One hospital reported a case where a patient waited 270 days for their NDIS application to be processed, only to pass away in the palliative care unit before receiving support.
Impact of NDIS Delays on Palliative Care
According to Palliative Care Australia, at least 5,000 people under the age of 65 are caught in funding gaps between the NDIS, the aged care system, and state health systems. These individuals often lack the necessary support to manage disabilities resulting from terminal illnesses. The situation is expected to worsen after November 1, when new Commonwealth regulations will restrict patients under 65 from moving into aged care homes.
Violet Platt, CEO of Palliative Care Victoria, emphasized the increasing reliance on the NDIS to find alternative arrangements for younger patients. “The consistent message I’m getting across the workforce is that palliative care patients are being prevented from going home because of the barriers in place trying to get an NDIS package,” she stated.
Personal Stories Highlight Systemic Issues
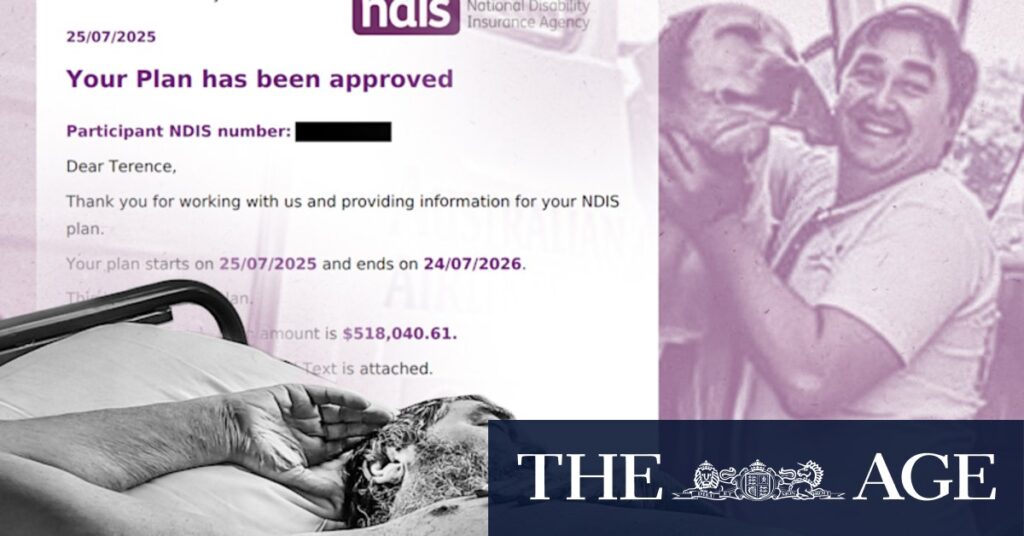
The story of Terry LeRoy, a former mechanic and racing enthusiast, underscores the challenges faced by many. After suffering a stroke and being diagnosed with late-stage liver cancer, Terry was left in a hospital bed for his final weeks, awaiting an NDIS grant that came too late. His mother, Doris LeRoy, described the situation as “ludicrous,” highlighting the emotional toll on families.
“He was lying naked on a bed in a stroke ward with just a nappy on,” Doris recounted. “It’s raw because he’s only just died, but there are absolutely other people in the same situation.”
Western Health’s chief operating officer, John Ferraro, expressed condolences to the LeRoy family and reiterated the hospital’s commitment to compassionate care. However, he noted that NDIS determinations are made by the NDIA, and the hospital works collaboratively with the agency to meet patients’ needs.
Challenges and Criticisms of the NDIS
A senior palliative care specialist, speaking anonymously, revealed that bed block is becoming more common for patients under 65, or under 55 if they are Aboriginal. These patients, who have significant time left to live, often have nowhere to go without an NDIS package. The specialist noted that the issue has arisen since the NDIS’s inception.
“We never used to have bed block in palliative care. It has been since the NDIS started,” the specialist said. “It’s basically younger people with significant disabilities, but who aren’t actively moving into an end-of-life care-type space.”
Palliative Care Victoria’s Violet Platt echoed these concerns, stating that some units are forced to discharge patients once an NDIS application is rejected, despite knowing they may soon return in more serious conditions.
“There’s been no inroads with NDIS, no clarity of the criteria,” Platt said. “Teams tell me they often feel that they’re set up to fail because they get to a point where there’s no more negotiation with the NDIS.”
Future Implications and the Need for Reform
The current situation highlights the urgent need for reform within the NDIS to address the gaps affecting terminally ill patients. The agency claims to have implemented a priority pathway for rapid eligibility testing and is focusing on improving the discharge process. However, the real-world impact remains to be seen.
As the healthcare system grapples with these challenges, the stories of individuals like Terry LeRoy serve as a stark reminder of the human cost associated with bureaucratic delays. The need for a more responsive and compassionate system is clear, and stakeholders are calling for immediate action to ensure that terminally ill patients receive the care and dignity they deserve in their final days.







