Australians suffering from one of the most prevalent forms of younger-onset dementia, known as behavioural-variant frontotemporal dementia (bvFTD), may be facing significant delays in diagnosis and treatment due to “overly restrictive” guidelines. This revelation comes from a comprehensive review conducted by researchers, which scrutinized the diagnostic criteria currently in use.
The study, led by Professor Olivier Piguet from the University of Sydney Brain and Mind Centre, suggests that the existing guidelines for diagnosing bvFTD could result in misdiagnoses, often confusing it with psychiatric disorders or other neurodegenerative diseases such as Alzheimer’s. This misdiagnosis not only delays appropriate treatment but also denies patients access to vital resources.
Understanding Frontotemporal Dementia
Frontotemporal dementia, which primarily affects individuals aged 45 to 65, is characterized by significant changes in behavior and personality, along with cognitive deficits. These deficits often impact executive functions like planning and decision-making, as well as social cognition. The condition is similar to primary progressive aphasia, a form of dementia that affects communication, famously diagnosed in actor Bruce Willis.
According to Professor Piguet, the current diagnostic criteria for bvFTD exclude many patients who clearly exhibit symptoms of the disease. “They will carry around an incorrect diagnosis potentially for months or years,” he stated, emphasizing the need for more inclusive guidelines.
A Personal Story: The Impact of Misdiagnosis
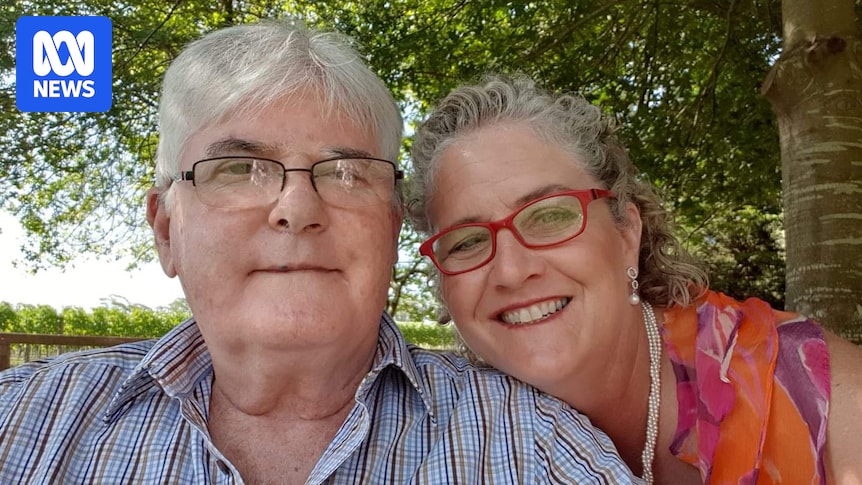
Julane Bowen, whose husband Jeff was diagnosed with bvFTD, shared her experience of watching her husband’s personality change drastically. Initially dismissed as effects of aging or mental health issues, Jeff’s symptoms were eventually recognized as bvFTD after a distressing incident led to his hospitalization.
“I had never heard of frontotemporal dementia but when I saw my husband’s brain scan, I came home and googled it,” Julane said. “I am reading the signs and symptoms and thinking, ‘Oh my god — he ticked every single box but one’. I couldn’t understand how the doctors could not actually see it.”
Julane’s story underscores the importance of timely and accurate diagnosis, which can significantly alter the trajectory of the disease for patients and their families.
Revising Diagnostic Criteria
The study, published in Alzheimer’s & Dementia, analyzed data from 110 patients over 14 years. It found that nearly 90% of patients presented with apathy or empathy loss, while only a small fraction met the criterion for cognitive dysfunction. By relaxing the definition of cognitive dysfunction, the number of qualifying patients increased dramatically.
“The research showed that behavioural symptoms were far more consistent and reliable indicators for bvFTD than current cognitive benchmarks,” Professor Piguet noted.
The researchers recommend revising the diagnostic criteria to remove the requirement for preserved memory and visuo-spatial skills, and to include social cognition as a core feature. This change acknowledges the significant impact of social functioning breakdowns in bvFTD patients.
Expert Opinions and Future Directions
Matthew Kiernan, a neurologist and chief executive of Neuroscience Research Australia, emphasized the need for further research and interdisciplinary discussion to refine diagnostic guidelines. “The good thing about this is that it is promoting discussion, and also trying to shift information across disciplines,” he said.
Similarly, Dr. Samantha Loi, a neuropsychiatrist at Royal Melbourne Hospital, highlighted the overlap between bvFTD and psychiatric conditions, suggesting that new criteria could benefit from incorporating biomarkers to aid differentiation.
While there is no cure for bvFTD, early and accurate diagnosis can provide a crucial window for intervention and support, improving quality of life for both patients and their families.
“It’s not that the person is being difficult — it’s a manifestation of the disease because of where the changes are in the brain,” Professor Piguet explained.
Julane Bowen’s experience with her husband Jeff, who continues to live a fulfilling life eight years post-diagnosis, illustrates the potential benefits of early intervention and tailored care strategies.
Conclusion: The Path Forward
The study’s findings highlight the urgent need for updated diagnostic criteria that better reflect the realities of bvFTD. By incorporating a broader range of symptoms and focusing on behavioral indicators, healthcare professionals can provide more accurate diagnoses and improve outcomes for patients.
As research continues, collaboration among global experts will be essential to develop guidelines that are both comprehensive and practical, ensuring that all patients receive the care and support they need.
If you or someone you know is affected by dementia, support is available through Lifeline, Beyond Blue, and the National Dementia Helpline.






