In a comprehensive review of qualitative studies, researchers have examined the task-technology fit (TTF) of Artificial Intelligence-based Clinical Decision Support Systems (AI-CDSSs) in healthcare. The analysis, which reviewed 21 case studies, sheds light on how these systems are being integrated into clinical decision-making processes and the challenges they face.
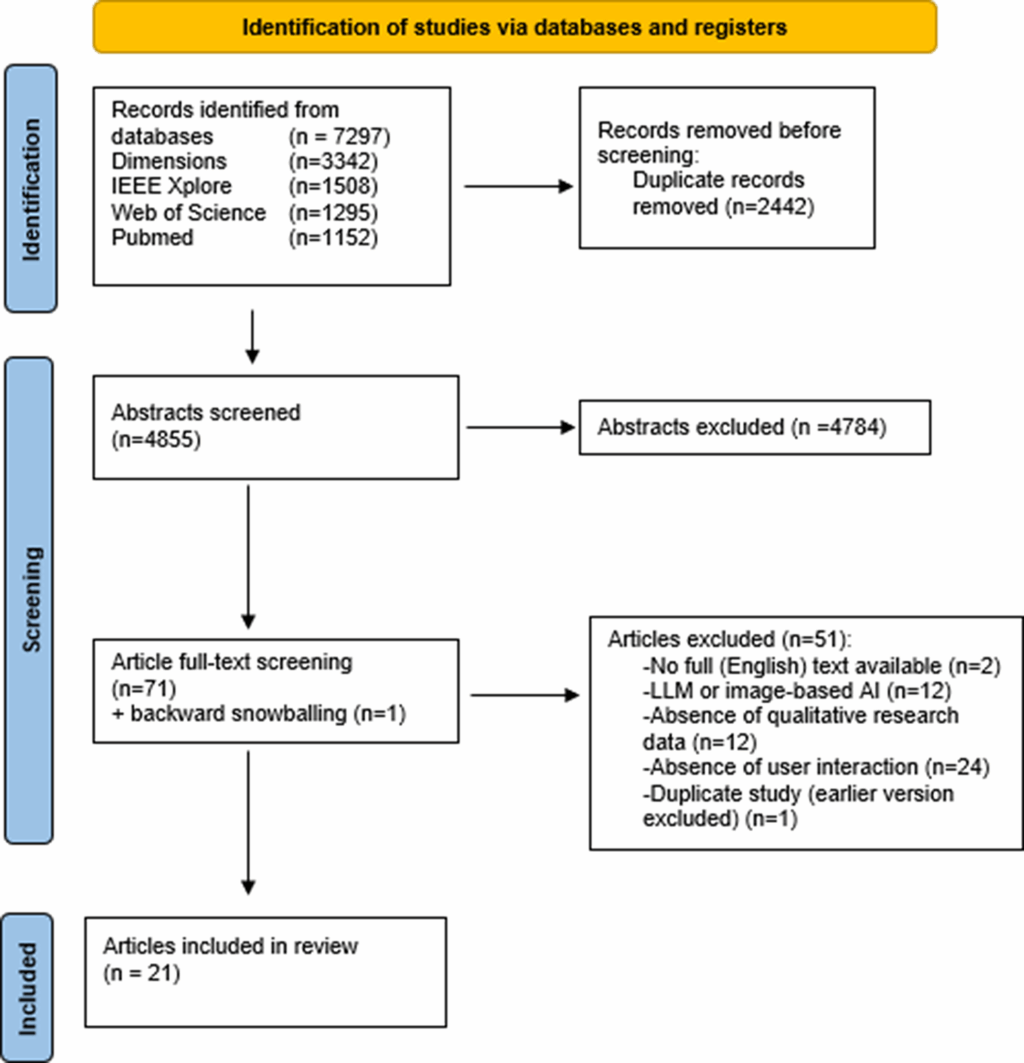
The review identified 7,297 studies, narrowing down to 4,855 unique ones after removing duplicates. Following a title and abstract screening, 72 studies were considered potentially relevant, with 21 meeting the inclusion criteria. Notably, nearly all studies were published post-2020, with a significant number conducted in the United States.
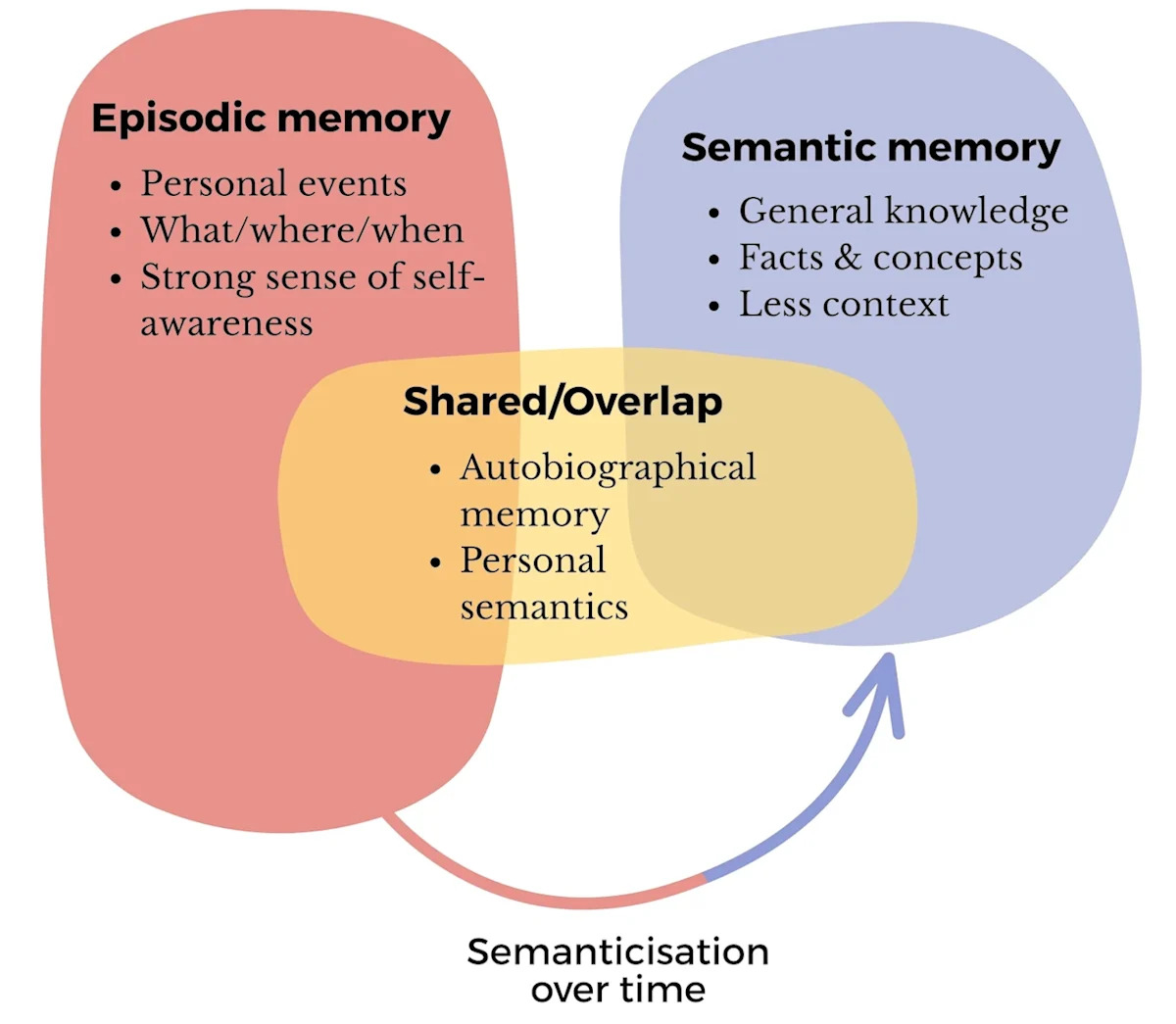
Understanding the Task-Technology Fit of AI-CDSSs
The analysis focused on various aspects that influence the TTF of AI-CDSSs, including technology-related characteristics, task characteristics, and individual clinician characteristics. A key finding was the maturity phase of AI-CDSSs, with most systems in the test phase, some implemented, and a few in the mock phase.
Technology Characteristics: Limitations and Needs
Despite the potential of AI-CDSSs to predict conditions such as delirium and sepsis, clinicians have encountered limitations in their application. A common issue was the interpretive challenge posed by percentage-based risk scores, which often lacked actionable insights for clinicians.
“So I’m not really sure what its goal is, but I can tell you that most of us ignore it (the sepsis risk score) because it has not proved helpful to what we do next.” — Emergency Room physician
To address this, some systems replaced percentage outputs with visual risk categorizations, which were more actionable and helped clinicians identify patients needing extra care. However, the need for AI recommendations to be directly applicable to clinical tasks was emphasized, with clinicians favoring systems that provided specific task recommendations.
Another significant limitation was the lack of access to key information, such as free-text notes and bedside observations, which are crucial for clinical decision-making. Clinicians also highlighted issues with data quality and the need for explainable AI (XAI) to provide insights into modifiable variables that influence prediction scores.
Strengths of AI-CDSSs
Despite these challenges, AI-CDSSs were acknowledged for their ability to process large volumes of data and detect subtle changes in patterns that clinicians might miss. Clinicians valued visualizations that improved prediction comprehension and appreciated the systems’ ability to explore different clinical actions and compare treatment strategies.
“Maybe the algorithm’s better at like kind of like nudging us to just like readdress some things that maybe are changing minutely day to day, so we may miss if we’re not, like, really aware of the trend.” — Physician
Task Characteristics: Opportunities and Challenges
Clinicians identified several areas where AI-CDSSs could enhance clinical practice, such as care acceleration, patient prioritization, and operational efficiency. These systems were particularly valued for their ability to facilitate risk communication and add objectivity to decision-making processes.
“The EWS triggers my mind to investigate a chart and see what’s going on and identifies patients to focus on, evaluate first, and decide if I need to intervene.” — Rapid Response Team clinician
However, the systems’ inability to fully account for patient complexity and individuality was a concern. Clinicians emphasized the need for AI-CDSS integration within electronic health records to access relevant clinical data and contextual information.
Individual Characteristics: Competencies and Cognitive Frameworks
The review highlighted individual differences in how clinicians perceive AI-CDSS recommendations, influenced by factors such as AI literacy and clinical expertise. While junior clinicians and non-specialists might benefit more from AI-CDSSs, some experienced clinicians expressed high confidence in their own judgment, occasionally disregarding AI recommendations.
“I feel like a lot of times we just kind of know when somebody is, like, not doing well, especially when we have the same patients often like day to day.” — Nurse
Clinicians’ evaluations of AI recommendations were also influenced by previous patient encounters, with a tendency towards recency bias. The role of intuition in clinical decision-making was particularly emphasized by senior clinicians.
Implications and Future Directions
The review concludes that while AI-CDSSs offer several opportunities to improve patient care, their potential is limited by challenges, particularly concerning integration into clinical workflows and the complexity of individual patients. Clinicians suggested that AI-CDSSs should complement their skills, such as identifying trends and integrating large amounts of data.
Moving forward, there is a need for more qualitative research to examine how clinicians’ TTF influences the use of AI-CDSSs. Future studies should also consider the long-term effects of AI-CDSSs on clinical practice, including their impact on intuition and expertise development.
Overall, the review underscores the importance of aligning AI-CDSS design with clinical tasks and the need for continuous monitoring and refinement to enhance task-technology alignment.