In a significant review of qualitative studies, researchers have delved into the task-technology fit (TTF) of Artificial Intelligence-based Clinical Decision Support Systems (AI-CDSSs). The review, which scrutinized 21 case studies involving clinicians’ interactions with AI-CDSSs, highlights the systems’ potential and limitations in enhancing clinical decision-making.
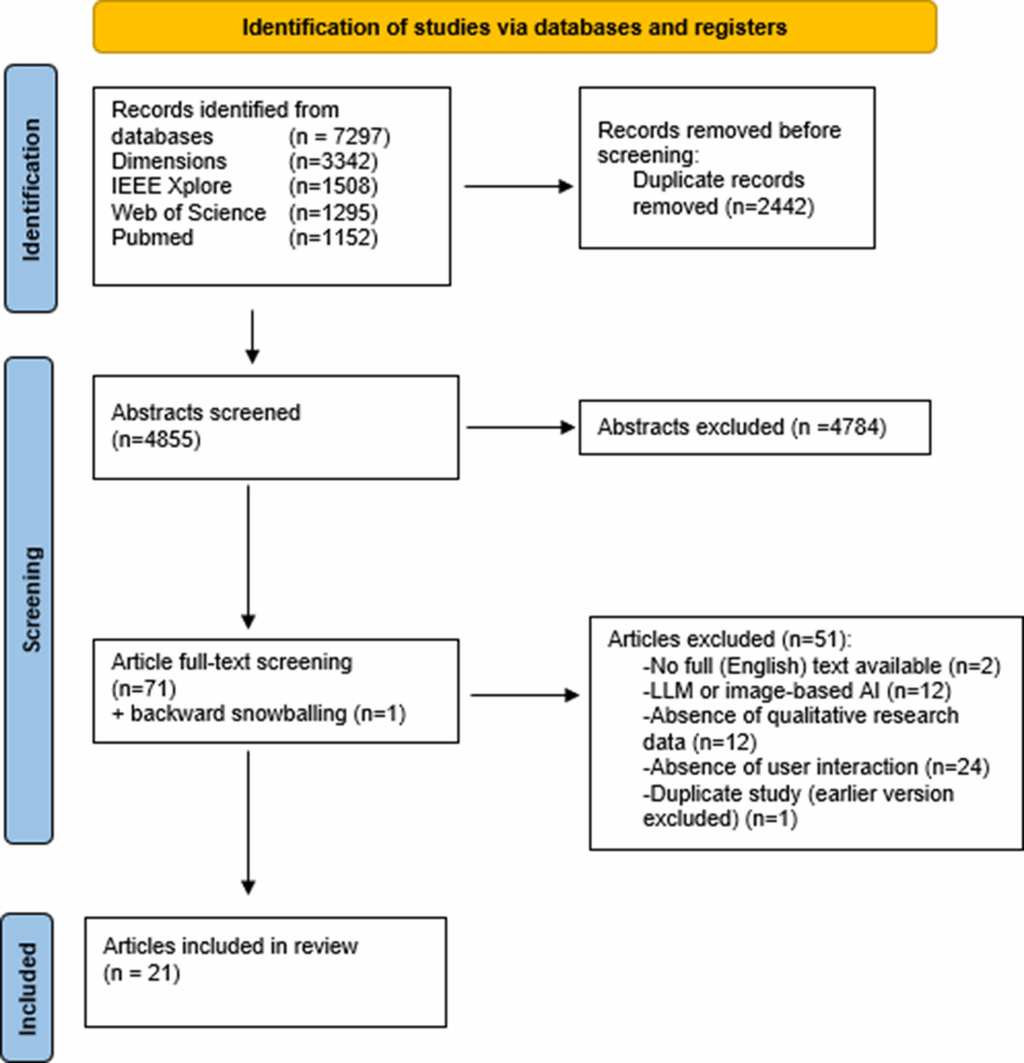
The review identified 7,297 studies, narrowing them down to 21 relevant case studies after rigorous screening. Notably, nearly all studies were published post-2020, with a majority conducted in the United States. The maturity phase of these AI-CDSSs varied, with most being in the test phase, followed by implemented and mock AI phases.
Technology Characteristics: Challenges and Adaptations
Despite the promise of AI-CDSSs in predicting conditions like delirium and sepsis, clinicians have encountered several limitations. A recurring issue is the interpretive challenge posed by percentage-based risk scores, which many clinicians found unhelpful in practical decision-making.
“So I’m not really sure what its goal is, but I can tell you that most of us ignore it (the sepsis risk score) because it has not proved helpful to what we do next.” – Emergency Room physician
In response, some systems have shifted to more intuitive visual risk categorizations, aiding clinicians in identifying patients needing urgent care. Additionally, clinicians expressed a need for AI recommendations to be directly applicable to their tasks, emphasizing the importance of actionable insights over granular data.
Another significant concern is the lack of access to crucial information such as free-text notes and bedside observations, which limits the AI’s effectiveness. Clinicians underscored the necessity for AI systems to integrate contextual data to enhance decision-making.
Task Characteristics: Opportunities and Efficiency
AI-CDSSs have shown potential in accelerating care and improving patient prioritization, particularly in resource-constrained environments. Clinicians have used these systems to identify early intervention opportunities, such as expedited ICU transfers and timely treatment for conditions like delirium.
“The EWS triggers my mind to investigate a chart and see what’s going on and identifies patients to focus on, evaluate first, and decide if I need to intervene.” – Rapid Response Team clinician
Furthermore, AI-CDSSs contribute to operational efficiency by facilitating rapid decision-making and reducing cognitive burdens. They also enhance risk communication among healthcare professionals, thereby improving treatment adherence and care coordination.
Individual Characteristics: Skills and Cognitive Frameworks
The review highlights individual differences in AI-CDSS usage, influenced by AI literacy, clinical expertise, and experiential anchoring. While junior clinicians and non-specialists may benefit more from AI-CDSSs, senior clinicians often rely on their intuition, sometimes disregarding AI recommendations entirely.
“I feel like a lot of times we just kind of know when somebody is, like, not doing well, especially when we have the same patients often like day to day.” – Nurse
Clinicians’ evaluations are also affected by recency bias, with recent patient encounters influencing their perception of AI recommendations. This variability underscores the need for tailored AI-CDSS designs that accommodate diverse clinical practices and expertise levels.
Implications and Future Directions
The review suggests that AI-CDSSs can enhance clinical decision-making by providing objective analyses and supporting data-driven insights. However, their effectiveness is limited by integration challenges and the complexity of individual patient cases.
To optimize AI-CDSSs, clinicians recommend flexible interfaces that prevent information overload and align with specific clinical needs. Integration with electronic health records (EHRs) is also crucial for accessing relevant contextual data.
Looking forward, the continuous evolution of AI-CDSSs requires ongoing assessment of task-technology alignment. As these systems adapt, they have the potential to refine clinical hypotheses and support diagnostic decisions, ultimately improving patient care.
In conclusion, while AI-CDSSs offer promising opportunities for enhancing clinical practice, their design and implementation must consider the unique needs and challenges of healthcare environments. Further research is essential to explore their long-term impact on clinical reasoning and decision-making.