The aging population across Europe is poised to significantly impact the burden of antimicrobial resistance (AMR), with older adults at heightened risk of serious bacterial infections. This growing concern underscores the urgency to implement effective strategies to combat AMR, as highlighted by a recent modelling study.
As populations age, the prevalence of infections resistant to antibiotics is expected to rise, complicating efforts to control AMR. The study emphasizes the need for policymakers to invest in evidence-based interventions and improve understanding of factors driving AMR rates. These efforts are crucial to meeting global targets, such as the 10% reduction in AMR mortality by 2030 set by the United Nations.
Understanding the Demographic Impact on AMR
Previous research has demonstrated that resistance prevalence in bloodstream infections (BSI) is significantly influenced by the age and sex of patients. For instance, methicillin resistance in Staphylococcus aureus (MRSA) tends to increase with age, affecting men more than women. Similarly, aminopenicillin resistance in Escherichia coli declines with age but remains higher in men. These patterns suggest that demographic factors must be considered in future AMR burden predictions.
Despite numerous studies indicating rising BSI rates, particularly among older adults and men, standardized estimates across Europe remain scarce. The study highlights the lack of clarity in previous AMR burden forecasts, often due to the omission of demographic shifts and variations in resistance by age and sex.
Modelling the Future Burden
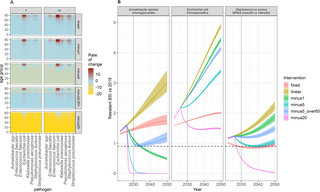
The study employs a comprehensive modelling approach to project future AMR burdens in Europe, considering demographic changes and resistance prevalence differences. By integrating data from the European Centre for Disease Control (ECDC), researchers aim to provide policymakers with robust estimates to inform intervention strategies.
Methodology
The study’s methodology involves three key steps: calculating projected BSI incidence rates, combining these with demographic projections, and using hierarchical modelling to estimate the number of antibiotic-resistant BSIs annually. The model assesses the impact of age and sex inclusion, projecting intervention impacts up to 2050.
Notably, the study focuses on three bacteria-antibiotic combinations: E. coli-aminopenicillin resistant, S. aureus-methicillin resistant, and Acinetobacter spp-aminoglycoside resistant. These were chosen due to their significant contribution to BSI etiology and substantial sample sizes.
Implications and Future Directions
The study’s findings indicate a projected increase in BSI incidence among older adults, particularly men, with substantial country-level variation in AMR burden projections to 2050. The research underscores the importance of accounting for demographic factors in resistance burden estimations, as failure to do so may lead to significant misestimations.
Even with successful public health interventions, 32% of the bacteria-antibiotic combinations studied may not achieve a 10% reduction in infection burden by 2030.
These projections highlight the need for targeted interventions, such as infection prevention control and antibiotic stewardship, to meet global AMR targets. The study also emphasizes the importance of stratified analyses to refine AMR burden estimates and intervention strategies.
Challenges and Opportunities
Long-term projections of AMR are inherently challenging due to the dynamic nature of resistance trends and demographic shifts. The study’s projections should be viewed as potential scenarios rather than forecasts, emphasizing the need for adaptive policy responses and continued global monitoring.
Future research should explore country-specific variations in resistance burden and the underlying drivers of age- and sex-related differences in BSI incidence. Understanding these factors could inform more precise intervention strategies and enhance predictive models.
Conclusion
The study provides a crucial advance in incorporating demographic shifts into AMR burden projections, offering a new approach to support policy discussions and decision-making. As Europe faces a rising resistance burden, immediate action is required to mitigate the anticipated challenges. Sustained efforts in surveillance, tailored interventions, and demographic-specific policy measures are essential to effectively combat AMR and reduce the future burden of bloodstream infections.
Ultimately, the findings underscore the importance of age and sex disaggregation in AMR burden assessments and the difficulty in achieving targets under expected demographic shifts. With robust data and strategic interventions, Europe can better navigate the complexities of AMR and safeguard public health for future generations.