Nairobi, Kenya — In a stark reminder of the intertwined challenges of drug abuse and HIV, Abdullahi Noor, a harm reduction advocate, recounts a haunting story of two brothers caught in the grip of addiction. Their tragic tale underscores a national crisis threatening Kenya’s ambitious goal to end new HIV infections and AIDS-related deaths by 2030.
The elder brother, deeply entrenched in heroin use, was secretly living with HIV. His younger sibling, desperate for a high, demanded to share a needle, ignoring warnings of HIV risk. The younger brother contracted HIV and succumbed to AIDS-related complications at 25, followed by his elder brother a year later, consumed by guilt and addiction.
Noor, who met the brothers while recovering from addiction himself, reflects, “Had that needle not been shared, perhaps they would still be alive. Two lives lost because of one needle. That is how unforgiving addiction is.”
Drug Abuse: A National Crisis
The tragic story of these brothers is emblematic of a broader crisis. Drug abuse is a significant barrier to Kenya’s fight against HIV. According to the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA), at least one in every six Kenyans aged 15 to 65 abuses drugs. Men are disproportionately affected, with one in three males using drugs, compared to one in 16 females.
The Coast region, notorious for heroin use and needle sharing, reports the highest rates of multiple drug use at 10.5%. Nairobi and Central regions follow closely. The use of cannabis has nearly doubled in the last five years, with Nairobi, Nyanza, and Coast recording the highest prevalence.
“At least two in every ten people who inject drugs in Kenya are HIV positive, further entrenching drug use as a driver of new infections,” experts warn.
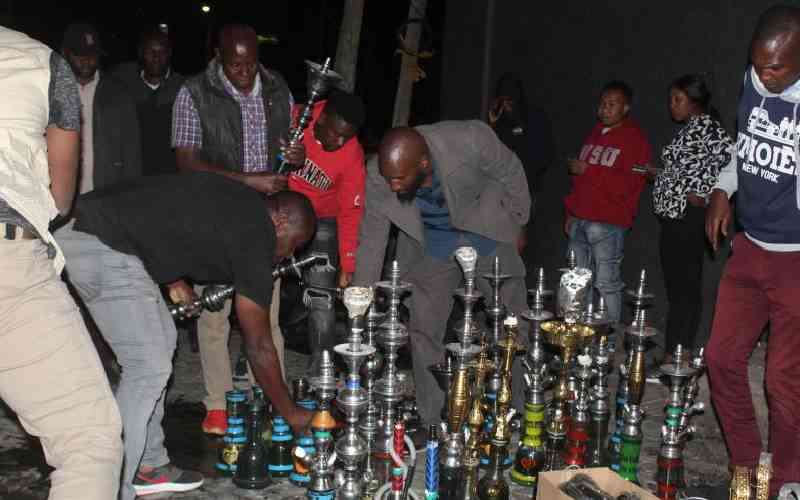
Efforts to Curb the Crisis
In response, the National Syndemic Diseases Control Council (NSDCC) is implementing harm reduction programs, including needle and syringe distribution to discourage sharing. “We supply needles and syringes to reduce the risk of infections. It is about minimizing harm while working toward rehabilitation,” says Douglas Bosire, acting CEO of NSDCC.
The program, in collaboration with NACADA and the National AIDS and STI Control Programme (NASCOP), also includes methadone therapy to help wean users off hard drugs. These efforts have reduced the proportion of new HIV infections from injecting drug use from 33% in 2011 to 13% in 2022.
“Despite these gains, many individuals undergoing rehabilitation struggle with reintegration and face social stigma,” Bosire notes.
Community and Policy Interventions
Efforts extend beyond harm reduction. NSDCC and NACADA are working with local leaders to foster community acceptance and inclusion. Programs focus on helping drug users overcome addiction and reintegrate into society, especially in coastal counties like Mombasa, Kwale, Kilifi, and Lamu.
Taib Abdulrahman, founder of Reach Out Center, attributes the high substance use in the Coastal region to drug trafficking through the Indian Ocean. “We have become a hub for heroin trafficking, witnessing horrifying scenes, overdoses, needle sharing, and broken families caused by drug and substance abuse,” he says.
Wangai Gachoka, manager of Miritini Rehabilitation Centre, emphasizes the need for comprehensive care, including distributing clean syringes, offering methadone, and providing free condoms to reduce HIV and hepatitis infections.
The Road Ahead
While heroin and cocaine remain significant threats, Gachoka warns of the rising abuse of miraa and muguka, particularly among youth aged 18 to 35. “These stimulants are cheap, legal, and easy to access, creating a dangerous cocktail when combined with other drugs,” he explains.
At Miritini, rehabilitation programs integrate psychosocial support, spiritual care, and vocational therapy to ensure holistic healing. Clients receive comprehensive care, including antiretroviral therapy (ART), PrEP, and treatment for TB, malaria, and hepatitis.
Gachoka believes that Kenya’s drug crisis requires more than treatment; it demands prevention and policy reform. “Accessibility is the biggest problem. If people didn’t have access to these drugs, fewer would be hooked,” he asserts.
As Kenya grapples with these challenges, the stories of individuals like Brian, a recovering addict at Miritini, highlight the potential for resilience and hope. Brian’s journey from addiction to advocacy underscores the importance of comprehensive support systems in combating drug abuse and its impact on HIV transmission.
Professor Omu Anzala, a virologist, stresses the need for proper disposal of medical waste to prevent needle reuse. “We are witnessing young men addicted to drugs hiding on streets, injecting themselves,” he laments.
The fight against drug abuse and HIV in Kenya is a complex battle requiring coordinated efforts across sectors. As the nation strives toward its 2030 goal, the stories of those affected by addiction serve as poignant reminders of the human cost of this crisis.







