Despite longstanding clinical guidelines cautioning against the practice, a significant portion of older Americans with dementia continue to be prescribed brain-altering medications. According to new research published in the journal JAMA on January 12, approximately one in four Medicare beneficiaries with dementia is prescribed these medications, which have been linked to increased risks of falls, confusion, and hospitalization.
While there has been a slight decline in the overall prescription rates of these medications among all Medicare beneficiaries—from 20% to 16% over a nine-year study period—they remain prevalent among individuals with cognitive impairments. This is particularly concerning given the heightened susceptibility of these patients to adverse effects.
Persistent Prescribing Patterns
Dr. John N. Mafi, senior author of the study and associate professor at the David Geffen School of Medicine at UCLA, highlighted the ongoing issue of inappropriate prescribing. “While this decline was encouraging, over two-thirds of patients receiving these prescriptions lacked a documented clinical indication in 2021, the end of the study period, suggesting high levels of potentially inappropriate and harmful prescribing,” he stated. “Compared with patients with normal cognition, we also found higher levels of prescribing among older adults with cognitive impairment, who face a higher risk of adverse effects from these drugs.”
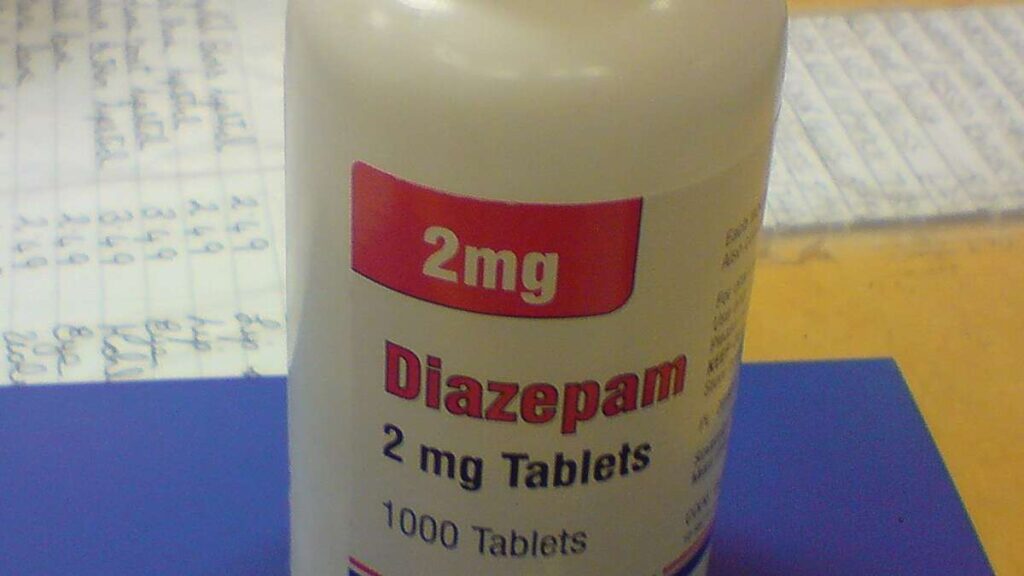
The study utilized survey data from the Health and Retirement Study, linked to Medicare fee-for-service claims, to analyze prescribing patterns of central nervous system (CNS)-active medications from 2013 to 2021. The medications in question include antidepressants with strong anticholinergic properties, antipsychotics, barbiturates, benzodiazepines, and non-benzodiazepine hypnotics.
By the Numbers
- CNS medications were prescribed to 17% of older adults with normal cognition.
- Nearly 22% of those with cognitive impairment but without dementia received these drugs.
- Approximately 25% of individuals with dementia were prescribed CNS-active medications.
Among all Medicare fee-for-service beneficiaries, the study noted specific trends in prescription rates:
- Benzodiazepines declined from 11.4% to 9.1%.
- Nonbenzodiazepine hypnotics fell from 7.4% to 2.9%.
- Antipsychotic prescriptions rose from 2.6% to 3.6%.
- Anticholinergic antidepressant prescriptions remained steady at 2.6%.
- Barbiturate prescriptions decreased slightly from 0.4% to 0.3%.
Implications and Recommendations
While the study highlights a decline in inappropriate prescriptions, driven largely by reductions in benzodiazepines and sleep medications, the persistence of these prescriptions raises concerns. Dr. Annie Yang, a scholar in the National Clinician Scholars Program at Yale University, emphasized the importance of careful medication management. “While CNS-active prescriptions may be appropriate in some cases, it is important for older patients or their caregivers to work closely with their physicians to ensure that these medications are appropriate to their cases,” she advised.
The study’s findings are limited by the lack of Medicare Advantage data and potential missing clinical information such as agitation. However, the research underscores the need for healthcare providers to consider alternative treatments and evaluate the safety of tapering or discontinuing these medications when deemed inappropriate.
Looking Forward
The research team, including co-authors from UCLA, RAND, and the University of Michigan, was funded by the National Institutes of Health/National Institute on Aging. As the population ages, the findings underscore a critical opportunity to enhance the quality and safety of care for millions of older Americans. Future efforts will likely focus on refining prescribing practices and ensuring that the use of CNS-active medications is both clinically justified and safe for patients with cognitive impairments.
As healthcare systems continue to evolve, the challenge remains to balance the benefits of these medications against their potential risks, particularly for vulnerable populations such as those with dementia. The study calls for ongoing education and collaboration among healthcare providers, patients, and caregivers to optimize treatment outcomes and safeguard patient health.





