Hypertension, a prevalent global health issue, is responsible for more than half of coronary artery diseases and two-thirds of strokes and heart failures worldwide. As of 2000, an estimated 972 million adults suffered from hypertension, with projections indicating a 60% increase to 1.56 billion by 2025. This alarming rise underscores the urgent need for effective intervention strategies.
The World Health Organization (WHO) has long emphasized the importance of controlling hypertension. In 2013, WHO’s World Health Day theme, “Measure your blood pressure, reduce your risk,” highlighted the necessity of preventing and managing high blood pressure. Despite these efforts, less than 25% of hypertensive patients achieve global disease control targets, pointing to gaps in awareness, adherence, and lifestyle choices.
Community-Based Interventions: A Promising Approach
Recent years have seen a growing recognition of community-based interventions as a viable strategy for hypertension prevention and control. These interventions engage local communities through health education, regular screenings, and referrals to health centers, aiming to raise awareness and promote self-management.
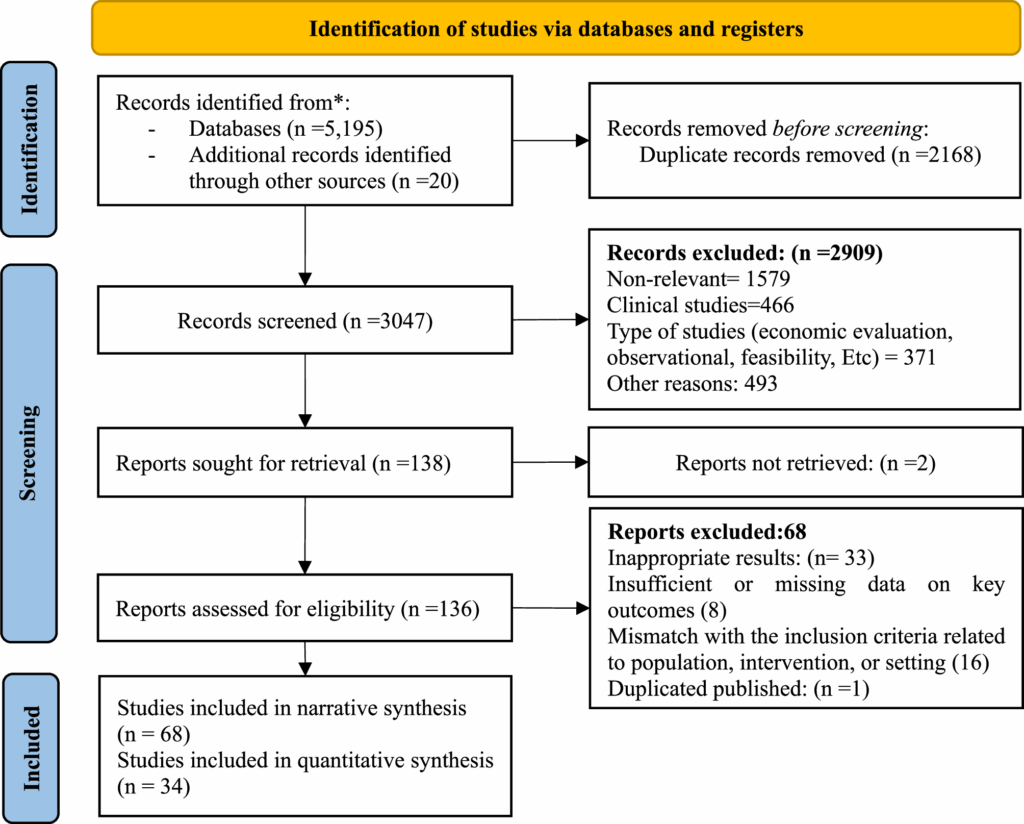
A systematic review and meta-analysis conducted in 2025 sought to evaluate the effectiveness of these interventions. The study followed rigorous guidelines, including the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and was registered in the International Prospective Register of Systematic Reviews (PROSPERO).
Methodology and Scope
The study analyzed data from 68 articles, including randomized controlled trials, quasi-experimental studies, and cohort studies. Researchers employed a comprehensive search strategy across databases such as PubMed, Scopus, and Web of Science, alongside manual searches in reputable journals and Google Scholar.
Inclusion criteria were based on the PICO framework, focusing on studies that assessed community-based interventions for hypertension control. The analysis revealed that interventions were most effective when conducted in healthcare settings, with significant reductions in both systolic and diastolic blood pressure.
Key Findings and Implications
The meta-analysis demonstrated that community-based interventions effectively reduced mean systolic and diastolic blood pressure. The interventions primarily included health education, lifestyle changes, increased physical activity, and dietary improvements.
“The greatest mean difference in systolic blood pressure was observed in interventions targeting individuals without hypertension, with a reduction of −8.26 mmHg,” the study reported.
Subgroup analyses indicated that interventions in healthcare settings were more effective than those in community or workplace settings. This effectiveness is attributed to better access to resources and expertise in healthcare environments, where continuous monitoring and follow-up are possible.
Challenges and Recommendations
Despite the promising results, the study identified several challenges. Educational interventions, though common, were less effective compared to lifestyle modification and dietary interventions. Barriers such as outdated communication methods and lack of participant engagement were noted.
To enhance effectiveness, the study recommends designing integrated and motivational educational interventions, utilizing trained local volunteers, and ensuring active participant engagement. Additionally, the study highlights the importance of tailoring interventions to the social, economic, and cultural contexts of target populations.
Future Directions and Considerations
While the study provides valuable insights, it acknowledges limitations such as language restrictions and high heterogeneity in intervention characteristics. Future research should consider including unpublished trials and grey literature to reduce potential publication bias and provide a more comprehensive understanding of intervention effectiveness.
Ultimately, the study underscores the potential of community-based interventions in hypertension control. By leveraging community resources and tailoring interventions to local contexts, health systems can effectively address this global health challenge.






