Schizophrenia, a complex neuropsychiatric disorder affecting approximately 1% of the global population, is often characterized by its hallucinatory and delusional symptoms. However, the disorder also manifests through “negative” symptoms such as profound apathy, reduced ability to experience pleasure, and progressive social withdrawal. These symptoms, which currently lack effective treatments, are particularly debilitating for those affected.
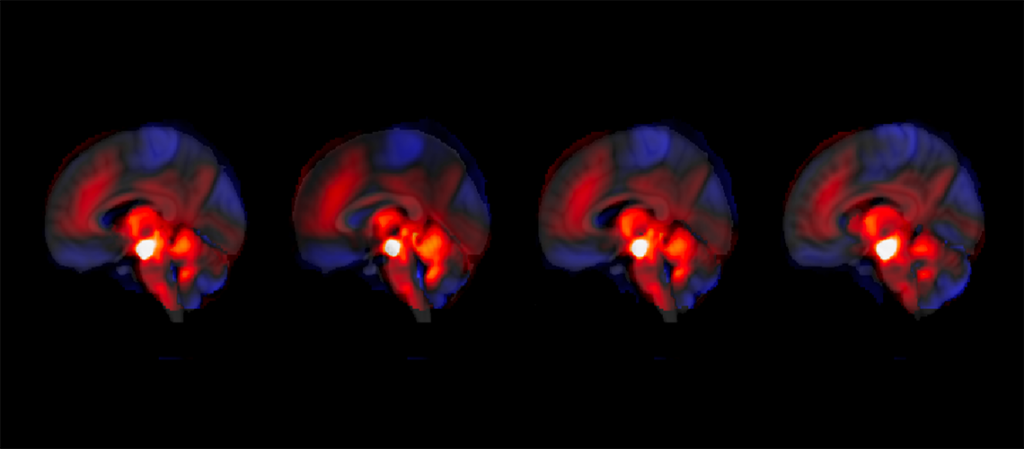
In a groundbreaking study, researchers have discovered a link between the cerebellum’s regulation of the brain’s reward system and the severity of these negative symptoms. Stronger cerebellar regulation is associated with a reduction in negative symptoms, while weaker regulation correlates with an increase in these symptoms.
The Cerebellum: More Than a Motor Function
Traditionally viewed as a region primarily responsible for motor control, the cerebellum is now being recognized for its significant emotional and cognitive roles. A team from the University of Geneva (UNIGE) and the Geneva University Hospitals (HUG) has demonstrated that the cerebellum plays a critical role in regulating the brain’s reward system, particularly through its interaction with the ventral tegmental area (VTA), a major dopamine-producing region.
“What is sometimes called our ‘little brain’ actually contains 50% of all our neurons,” explains Indrit Bègue, assistant professor in the Laboratory of Neuroimaging and Translational Psychiatry at the UNIGE Faculty of Medicine. “Although it was long considered to have a purely motor function, we are now discovering that it also plays important emotional and cognitive roles.”
Understanding the Reward System
Abnormalities in the brain’s reward system, especially within the VTA, have been linked to the negative symptoms of schizophrenia. In individuals with the disorder, the VTA is believed to be overactive, leading to a blunted perception of salience, where “everything feels the same,” resulting in a lack of motivation.
The study by UNIGE and HUG researchers involved following 146 patients over a period of 3 to 9 months, as well as analyzing an independent validation cohort. This comprehensive approach allowed them to observe and describe the functional connection between the cerebellum and the VTA in the context of schizophrenia for the first time.
Implications for Treatment
The findings of this study open new avenues for targeted therapeutic interventions. “We show that stronger cerebellar regulation of the reward system is associated with a reduction in negative symptoms — and conversely, weaker regulation with an increase in symptoms,” explains Jade Awada, a doctoral student and first author of the study.
The analyses were carried out by Jade Awada and Farnaz Delavari, co-first author of the study and researcher in Professor Stephan Eliez’s laboratory. Their work suggests that the cerebellum could become a more accessible therapeutic target for treating the negative symptoms of schizophrenia.
Future Research Directions
The study’s results represent a significant step forward in understanding the complex mechanisms of schizophrenia. Future research could focus on developing therapies that enhance cerebellar regulation of the reward system, potentially offering relief for symptoms that have long been considered intractable.
According to experts, these findings could also pave the way for broader investigations into the cerebellum’s role in other neuropsychiatric disorders, further expanding our understanding of this often-overlooked brain region.
As research continues, the hope is that these insights will lead to more effective treatments, improving the quality of life for individuals living with schizophrenia and potentially transforming the approach to managing this challenging disorder.