Researchers have made a significant breakthrough in personalized medicine by discovering a method to predict which lung cancer patients will respond to costly immunotherapy treatments. This innovation could potentially transform treatment protocols and improve patient outcomes.
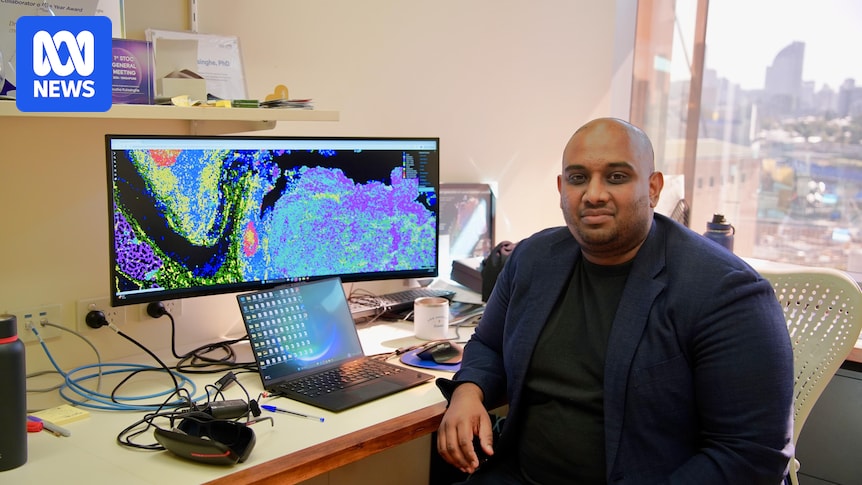
University of Queensland researcher Arutha Kulasinghe spearheaded a study involving lung biopsies from nearly 250 patients with non-small cell lung cancer across Australia, the United States, and Europe. Non-small cell lung cancer is the most prevalent form, affecting approximately 90% of patients. Collaborating with scientists in the US and Melbourne, Associate Professor Kulasinghe utilized advanced microscopes and computational analysis to examine millions of cells in each sample.
“We wanted to find out if there were patterns in the tissues that were predictive of response or resistance to immunotherapies,” Kulasinghe explained. The study, likened to a “Google Maps approach” to cancer analysis, revealed that the spatial arrangement and interaction of certain cells could predict patient responses to the immunotherapy drug Keytruda.
Mapping Cell Patterns
Keytruda is effective in only 20 to 30% of lung cancer patients, a sobering statistic considering lung cancer remains the leading cause of cancer-related deaths globally, claiming around 9,000 lives annually in Australia alone. The financial burden of immunotherapy is substantial, with annual costs ranging from $400,000 to $500,000 per patient, and it can be highly toxic for some individuals.
Professor Kulasinghe, based at UQ’s Frazer Institute, described how the research team mapped every cell within a patient’s biopsy, each containing between three to five million cells. By employing artificial intelligence, they mined the samples for data to “understand patterns associated with response and resistance to therapy.”
The researchers identified a “molecular fingerprint” within the cancer samples that could predict a patient’s response to immunotherapy treatments. “Certain immune cells are in close proximity to tumor cells in patients that do well on immunotherapy, and those patterns are crucial to profile and screen for,” Kulasinghe noted, emphasizing the consistency of these patterns across different geographic locations.
“Those become potentially useful signatures that we can start using to screen populations of lung cancer patients,” he added.
Potential for New Treatments
The research, published in the scientific journal Nature Genetics, holds promise for developing new treatments that could be combined with immunotherapy to enhance patient response. Professor Kulasinghe’s passion for cancer research traces back to his childhood, inspired by his grandfather’s battle with colorectal cancer.
Almost three decades later, lung cancer advocate Michel Itel hailed Kulasinghe’s work as revolutionary. Diagnosed with advanced lung cancer in 2017, Itel has firsthand experience with the disease’s challenges. “I don’t light up like a Christmas tree with my scans,” he said, referring to his current treatment’s effectiveness.
As a research advocate, Itel travels globally to stay abreast of the latest advancements. “I think it’s definitely going to be a game changer in how we do disease analysis,” he remarked, viewing the research as a beacon of hope rather than just a scientific endeavor.
The Right Treatment for the Right Patient
Lung Foundation Australia CEO Mark Brooke described the study as “an incredible breakthrough in lung cancer.” He emphasized the importance of targeting the right treatment to the right patient at the right time, a strategy that this new research supports.
“Increasingly, lung cancer is treated by targeting the right treatment to the right patient at the right time, so this new way of looking at lung cancers is quite exciting for the patient community,” Brooke said.
“There are researchers working on different parts of the lung cancer puzzle, right across the world. It is a time for optimism and hope,” he added.
Smoking Not the Only Cause
Professor Kulasinghe’s study included both smokers and non-smokers, challenging the stigma that lung cancer is solely a smoking-related disease. “It’s really important that we challenge the stigma and the biases associated with smoking-related illnesses,” Brooke stated.
An emerging group of lung cancer patients has never smoked, highlighting other risk factors such as family history and environmental exposure. “It could be family history, it could be where you work and how you work,” Brooke explained.
Advancements in precision medicine and targeted therapies have significantly improved the five-year survival rate for lung cancer patients from about 16% a decade ago to 26% today. “Lung Foundation Australia set out to see the five-year survivorship rate increase to 50% by 2030, and I think if you look at the global trends, we are absolutely on track,” Brooke concluded.





