In a groundbreaking development, researchers have successfully created human eggs from skin cells, potentially revolutionizing in vitro fertilization (IVF) treatments. This advancement, achieved by scientists at Oregon Health and Science University in Portland, could offer new hope for couples facing infertility due to age, illness, or medical treatments.
The research, while still in its early stages, holds the promise of providing genetically related eggs for women who are infertile. Moreover, the same technique could be adapted to benefit same-sex male couples by creating eggs from male skin cells. “The largest group of patients who might benefit would be women of advanced maternal age,” stated Prof. Shoukhrat Mitalipov, who led the research team. “Another group are those who have been through chemotherapy because that can affect their ability to have viable eggs.”
The Science Behind the Breakthrough
The process draws on cloning techniques pioneered in the 1990s at the Roslin Institute in Scotland, where somatic cell nuclear transfer was used to create Dolly the sheep. The Oregon team employed a similar approach, extracting nuclei from skin cells and inserting them into donor eggs that had their own nuclei removed. This intricate procedure aims to mimic the natural fertilization process.
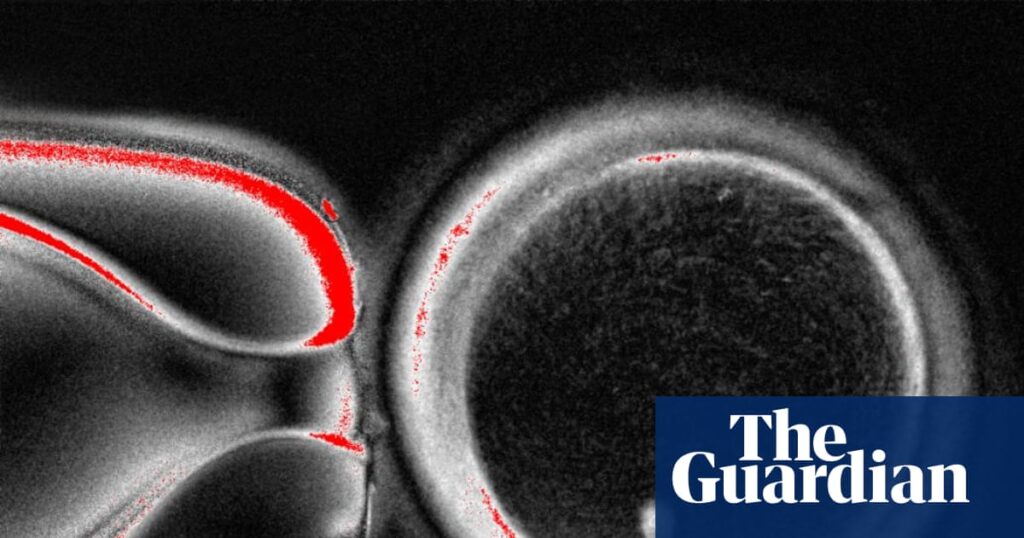
One of the significant challenges faced by the researchers was the discrepancy in chromosome numbers. Human eggs naturally contain 23 chromosomes, which pair with another 23 from sperm during fertilization. The team addressed this by using a compound called roscovitine, which helped the eggs adjust their chromosome count appropriately. However, the initial results showed that the chromosomes paired up randomly, leading to embryos with incorrect chromosome numbers.
Challenges and Future Prospects
Despite the promising nature of this research, the process is not yet efficient. Out of 82 eggs created, less than 10% reached the stage suitable for IVF embryo transfer, and none were cultured beyond six days. Prof. Paula Amato, a co-author of the study, noted that “these abnormal chromosome complements would not be expected to result in a healthy baby.” The team is actively working on refining the technique to improve its efficiency and safety.
Prof. Mitalipov described the work as a “proof of concept,” acknowledging the significant challenges that lie ahead. “I think it’s going to be harder than what we’ve done over the years thus far, but it’s not impossible,” he remarked, estimating that perfecting the technique could take another decade.
Expert Opinions and Ethical Considerations
The breakthrough has garnered praise from the scientific community. Prof. Richard Anderson from the University of Edinburgh emphasized the potential impact on women who have lost their eggs due to various reasons, including cancer treatment. “The ability to generate new eggs would be a major advance,” he said, while also highlighting the importance of addressing safety concerns.
Prof. Ying Cheong of the University of Southampton noted the increasing number of patients unable to use their own eggs due to age or medical conditions. She suggested that this early laboratory work could eventually transform our understanding of infertility and miscarriage, potentially leading to new options for those without viable reproductive cells.
Meanwhile, Prof. Roger Sturmey of the University of Hull praised the scientific achievement but stressed the necessity for open dialogue with the public. “Breakthroughs such as this impress upon us the need for robust governance, to ensure accountability and build public trust,” he commented.
Implications for the Future of Fertility Treatments
This development represents a significant step forward in reproductive medicine, potentially expanding the possibilities for individuals and couples facing infertility. If perfected, the technique could provide a genetic link for those who previously had no options. However, the path to clinical application is fraught with technical and ethical challenges that must be navigated carefully.
As the research progresses, scientists and ethicists alike will need to address the broader implications of creating eggs from skin cells. The potential to alter the landscape of fertility treatments is immense, but so too is the responsibility to ensure these advancements are safe, ethical, and accessible.
The next decade will be crucial in determining whether these laboratory successes can translate into viable treatments, offering hope to many who dream of starting a family.