Over the past two decades, CD40 agonist antibodies have been at the forefront of cancer research, promising to revolutionize treatment by activating the immune system to target cancer cells. Despite their potential, these drugs have often fallen short in clinical trials, causing severe side effects such as systemic inflammation, low platelet counts, and liver toxicity, even at minimal doses. However, a recent breakthrough from Rockefeller University’s Jeffrey V. Ravetch has reignited hope in this field.
In 2018, Ravetch’s lab engineered an enhanced CD40 agonist antibody, named 2141-V11, which demonstrated increased efficacy and reduced side effects in animal models. This engineered antibody was designed to bind more effectively to human CD40 receptors and was administered directly into tumors to minimize systemic toxicity. The promising results from these preclinical studies led to a phase 1 clinical trial to evaluate its impact on human cancer patients.
Clinical Trial Results: A New Hope for Cancer Patients
The results of the phase 1 clinical trial, recently published in Cancer Cell, are nothing short of remarkable. Of the 12 patients involved, six experienced tumor shrinkage, with two achieving complete remission. “Seeing these significant shrinkages and even complete remission in such a small subset of patients is quite remarkable,” stated Juan Osorio, the study’s first author and a medical oncologist at Memorial Sloan Kettering Cancer Center.
Notably, the drug’s effects were not limited to the injected tumors; other tumors in the body also shrank or were eliminated by immune cells. This systemic response from a localized injection is a rare and unexpected outcome in clinical treatments, adding to the excitement surrounding 2141-V11.
Engineering Enhancements: A New Approach to CD40 Agonists
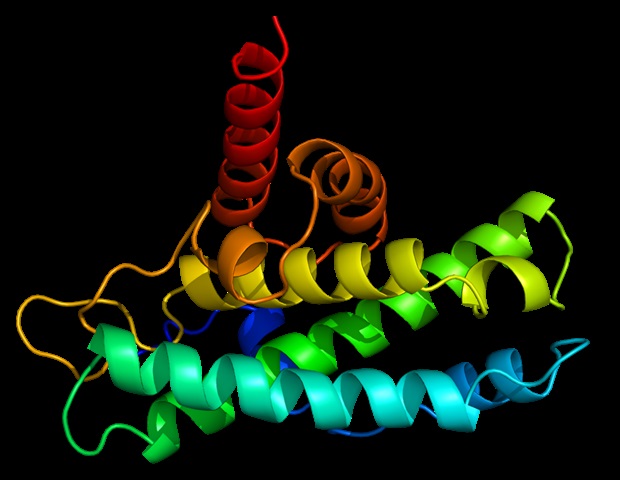
CD40, a cell surface receptor, plays a crucial role in activating the immune system. Ravetch’s lab, supported by Rockefeller’s Therapeutic Development Fund, engineered the 2141-V11 antibody to enhance its binding to CD40 receptors and improve its ability to initiate an immune response. By modifying the antibody to engage a specific Fc receptor, they increased its potency tenfold.
Traditionally, CD40 agonists were administered intravenously, leading to widespread uptake by non-cancerous cells and resulting in toxic side effects. Ravetch’s team instead injected the antibody directly into tumors, significantly reducing toxicity. “When we did that, we saw only mild toxicity,” Ravetch noted, underscoring the importance of administration method in drug efficacy.
Inducing Remission: A Closer Look at the Trial
The trial included patients with various metastatic cancers, including melanoma and breast cancer. Remarkably, none of the participants experienced the severe side effects typical of other CD40 drugs. Among the six patients who saw systemic tumor reduction, two achieved complete remission, with their cancers disappearing entirely.
One patient with melanoma had multiple metastatic tumors, yet only one tumor was injected, resulting in the disappearance of all tumors. Similarly, a breast cancer patient with tumors in multiple organs saw complete remission after the injection of a single skin tumor. Tissue analysis revealed that the drug stimulated a robust immune response, transforming tumors into immune cell-rich environments resembling lymph nodes.
“We were quite surprised to see that the tumors became full of immune cells-including different types of dendritic cells, T cells, and mature B cells-that formed aggregates resembling something like a lymph node,” Osorio explained.
Improving Immunotherapy: Future Directions
The success of 2141-V11 has spurred additional clinical trials in collaboration with researchers at Memorial Sloan Kettering and Duke University. These trials, now in phase 1 or phase 2, are exploring the antibody’s effects on aggressive cancers such as bladder cancer, prostate cancer, and glioblastoma, with nearly 200 participants enrolled.
These studies aim to uncover why some patients respond to 2141-V11 while others do not, and how to enhance its efficacy. Preliminary findings suggest that patients with a high clonality of T cells, which are key to attacking cancer cells, are more likely to respond to the treatment.
“As a general rule, only 25 to 30% of patients will respond to immunotherapy, so the biggest challenge in the field is to try to determine which patients will benefit from it,” Ravetch stated. “What are the indicators or predictors of response? And how can we convert non-responders into responders?”
The breakthrough with 2141-V11 represents a significant advancement in cancer immunotherapy, offering new hope for patients with hard-to-treat cancers. As research continues, the potential to refine and expand the use of engineered antibodies could transform the landscape of cancer treatment.