Researchers at McMaster University, Cleveland Clinic, and Case Comprehensive Cancer Center have made a groundbreaking discovery linking a protein traditionally associated with Alzheimer’s disease to the spread of lung cancer to the brain. This revelation presents an opportunity to repurpose existing Alzheimer’s medications to potentially curb cancer metastasis.
The study, published in Science Translational Medicine on July 2, 2025, focuses on the protein BACE1, which is instrumental in the formation of brain metastases in lung cancer patients. These metastases occur in up to 40 percent of individuals suffering from non-small cell lung cancer.
“We’ve always associated BACE1 with Alzheimer’s disease, so to find it playing a major role in lung cancer brain metastases is an important discovery. It’s a reminder that cancer can hijack biological pathways in ways we don’t yet fully understand,” said Sheila Singh, senior author and director of McMaster’s Centre for Discovery in Cancer Research.
Unveiling BACE1’s Role in Cancer
To uncover BACE1’s role in cancer spread, researchers employed a sophisticated gene activation technique known as a genome-wide in vivo CRISPR activation screen. This method allowed them to activate thousands of genes in lung cancer cells systematically, which were then introduced into mice. The activation of BACE1 significantly increased the likelihood of cancer cells invading the brain.
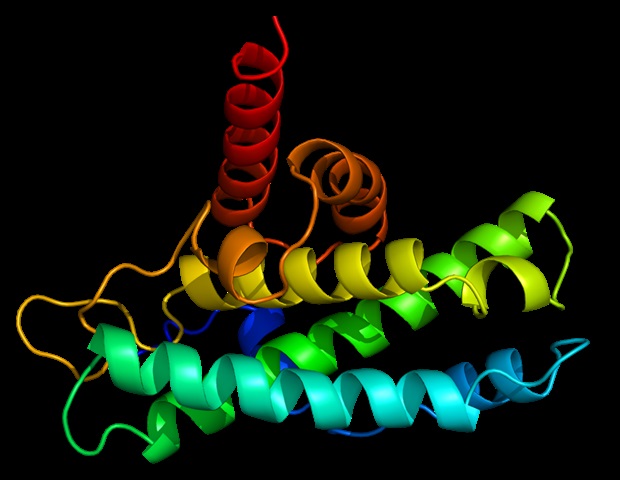
BACE1 is well-known in Alzheimer’s research for its role in cutting the APP protein, leading to the formation of amyloid plaques in the brain. This connection to cancer metastasis opens new avenues for therapeutic interventions.
Repurposing Alzheimer’s Drugs
Currently, treatment options are limited once cancer spreads to the brain. However, the discovery of BACE1’s involvement provides hope that Alzheimer’s drugs could be repurposed. One such drug, Verubecestat, which inhibits BACE1 activity, showed promising results in animal studies. Mice treated with Verubecestat developed fewer and smaller tumors and had extended survival rates.
“The discovery of BACE1 opens the door to repurposing existing treatments like Verubecestat to potentially prevent or slow the spread of lung cancer to the brain, where treatment options are currently very limited,” Singh noted.
Despite its initial promise in Alzheimer’s treatment, Verubecestat’s Phase 3 clinical trial was halted in 2018 due to an unfavorable benefit-risk assessment. This new research could reignite interest in its potential applications for cancer therapy.
Future Research and Implications
The research team emphasizes the need for further studies to fully understand the effectiveness of BACE1-targeted therapies in preventing lung cancer from spreading to the brain. This discovery underscores the importance of interdisciplinary collaboration in advancing treatment for complex diseases.
“This study highlights how interdisciplinary partnerships can lead to breakthroughs in understanding and treating devastating diseases like brain metastases,” said Shideng Bao, a researcher at Cleveland Clinic and a corresponding author on the paper.
The collaboration between McMaster University, Cleveland Clinic, and Case Comprehensive Cancer Center continues to push the boundaries of cancer research, with Singh and her colleagues being recognized as leaders in the field. Their previous work has already identified pathways used by cancer cells to infiltrate the brain, paving the way for innovative therapeutic approaches.
The study received support from various organizations, including the Boris Family Fund for Brain Metastasis Research, the Canadian Cancer Society, and the Cancer Research UK Lung Cancer Centre of Excellence, among others.
As the scientific community delves deeper into the relationship between BACE1 and cancer metastasis, the potential for repurposing Alzheimer’s drugs offers a beacon of hope for patients facing the grim prognosis of brain metastases.







