In a groundbreaking study published in Lancet Digital Health, researchers from Stanford Medicine have developed a machine learning-based model that could significantly enhance the efficiency and cost-effectiveness of liver transplants. The model, which predicts whether a donor is likely to die within the critical time frame for organ viability, has the potential to transform the transplant landscape by reducing futile procurements by 60%.
The announcement comes as the demand for liver transplants continues to outpace the supply of available organs. Despite the growing number of candidates on the waitlist, about half of the potential transplants are canceled when a donor dies too late after cardiac arrest following the removal of life support. This issue is particularly pertinent in cases of donation after circulatory death, where the time between life support removal and death must not exceed 30 to 45 minutes to ensure the organ’s viability.
Revolutionizing the Transplant Process
According to Dr. Kazunari Sasaki, clinical professor of abdominal transplantation and senior author of the study, the new AI model provides a solution by predicting the likelihood of a donor’s death occurring within the viable time frame. “By identifying when an organ is likely to be useful before any preparations for surgery have started, this model could make the transplant process more efficient,” Sasaki explained. “It also has the potential to allow more candidates who need an organ transplant to receive one.”
The research, led by Rintaro Yanagawa of Kyoto University, highlights the model’s ability to outperform traditional surgeon judgment. The AI model was trained on over 2,000 real-world cases from six U.S. transplant centers, demonstrating a 75% accuracy rate in predicting the donor’s time of death, compared to the 65% accuracy rate of surgeons.
Enhancing Donation After Circulatory Death
For patients with end-stage liver disease, a transplant often represents the best treatment option. However, the number of donors remains insufficient. Recent advancements, such as normothermic machine perfusion, have started to bridge this gap by preserving organs at an optimal temperature during transportation, thereby increasing the viability of donations after circulatory death.
“The number of liver transplants keeps going up because of donation after circulatory death, and the waitlist is getting smaller,” Sasaki noted. “In the future, it might be possible for everyone who needs a liver transplant to get one from a deceased donor.”
Despite these advancements, donation after circulatory death presents challenges, primarily due to the time-sensitive nature of organ viability. The AI model addresses these challenges by utilizing a comprehensive array of clinical data, including the donor’s vital signs, blood work, and neurological assessments, to predict the time of death more accurately.
Competing Algorithms and Future Prospects
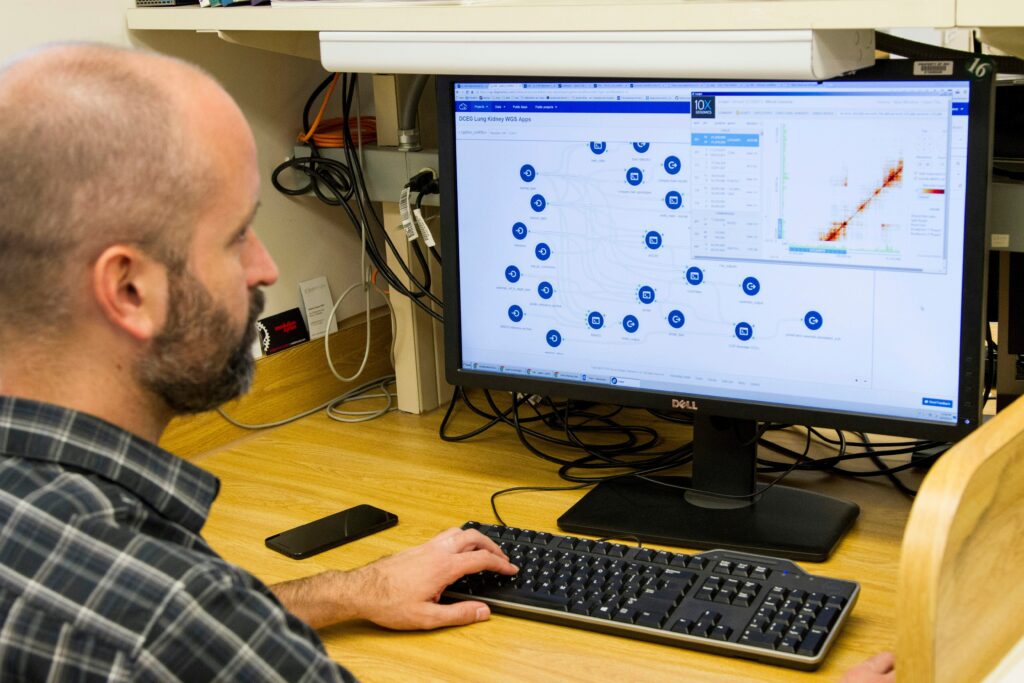
The research team meticulously compared various machine-learning algorithms to identify the most effective one for predicting time of death. The chosen algorithm not only surpassed existing tools but also proved adaptable to different surgeon preferences and hospital procedures. This adaptability is crucial for integrating the model into diverse clinical settings.
The model’s design includes a natural language interface, akin to ChatGPT, which extracts relevant information from donor medical records. This feature streamlines the process, ensuring that critical data is readily accessible for decision-making.
Despite its success, the model shares a similar rate of missed transplant opportunities with surgeon judgment, both hovering just over 15%. However, the rapid advancement of artificial intelligence offers hope for further improvements. “We are now working on decreasing the missed opportunity rate because it is in the patients’ best interest that those who need transplants receive them,” Sasaki stated. “We continue to refine the model by having competitions among available machine learning algorithms, and we recently found an algorithm that achieves the same accuracy in predicting the time of death but with a missed opportunity rate of about 10%.”
Broader Implications and Collaborations
The implications of this study extend beyond liver transplants. The research team is exploring variations of the model for use in heart and lung transplants, potentially revolutionizing these fields as well. This collaborative effort involved contributions from several prestigious institutions, including the International University of Health and Welfare, Duke University School of Medicine, and the Cleveland Clinic, among others.
As the model continues to evolve, it represents a significant step forward in transplant medicine, offering hope to thousands of patients awaiting life-saving organ transplants. The integration of advanced AI technology into clinical practice not only promises to enhance the efficiency of the transplant process but also underscores the transformative potential of machine learning in healthcare.