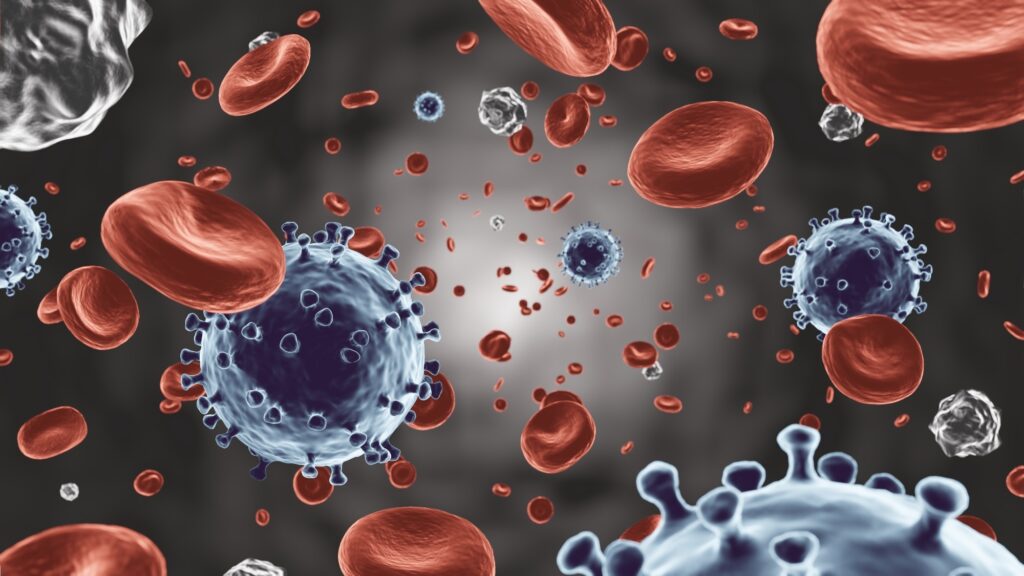
A groundbreaking international study has revealed that COVID-19 survivors, particularly women, exhibit signs of accelerated vascular aging. This alarming discovery, however, comes with a silver lining: early evidence suggests that some of this vascular damage may be reversible over time.
Published in the European Heart Journal, an editorial delves into the implications of COVID-19 on vascular health, suggesting that the pandemic has left a lasting imprint on the vasculature akin to accelerated aging. This phenomenon is framed within the context of post-acute COVID-19 syndrome (PACS), a condition defined by the World Health Organization (WHO) as symptoms persisting for at least two months after the initial three-month post-infection period.
Understanding the Impact of COVID-19 on Vascular Health
The editorial highlights the CARTESIAN cohort study, which included both asymptomatic and symptomatic COVID-19 survivors. Notably, the study did not strictly adhere to the WHO criteria for PACS. The cardiovascular symptoms observed range from dysautonomia and microvascular vasospasm to more severe conditions like myocardial infarction and venous thromboembolism. These are thought to be linked to endothelial injury, inflammation, and coagulation disturbances.
Key questions arise from these findings: Can these injuries be objectively measured? How do they relate to the severity of the disease? Which groups are most vulnerable, and how long do these effects persist?
Findings from the CARTESIAN Cohort
The CARTESIAN cohort study stands out for its comprehensive scope and analytical rigor. It enrolled 2,390 participants across 34 centers, categorizing them into COVID-19-negative controls and COVID-19-positive individuals, further divided based on hospitalization status. At a six-month follow-up, adjusted arterial stiffness, measured by carotid–femoral pulse wave velocity (PWV), was significantly higher in all COVID-19-positive groups compared to controls.
By the Numbers: Using an adjusted control PWV of 7.53 m/s as a reference, the absolute differences were +0.41 m/s (non-hospitalized), +0.37 m/s (hospitalized), and +0.40 m/s (ICU).
Interestingly, while a severity gradient was expected, the data did not show a clear linear increase in stiffness from non-hospitalized to ICU levels. However, sex-stratified models revealed a distinct pattern: women across all COVID-19-positive groups had elevated PWV, with the most significant increase observed in those requiring ICU care.
Sex Differences and Mechanistic Insights
The editorial raises critical questions about the differential impact of COVID-19 on women’s cardiovascular health. It suggests that women’s hearts might respond differently to the increased workload caused by stiffer arteries post-COVID-19. The CARTESIAN study’s methodological strengths, such as its large, international sample and validated surrogate for vascular aging, lend credibility to these findings.
Furthermore, 12-month data from the study indicate that while controls showed expected age-related PWV progression, many COVID-19 survivors experienced a decline in PWV over time. This suggests that part of the stiffness signal may diminish as autonomic imbalance and inflammation subside.
“The editorial interprets these dynamics as consistent with a composite injury in which some components are transient while others likely represent irreparable damage.”
Exploring the Underlying Biology
The editorial explores the biological mechanisms that might explain these sex-specific findings. It discusses the potential role of hormonal influences, such as estrogen’s effects on endothelial function, and social determinants like differential exposure and access to care. The inflammatory milieu of COVID-19, characterized by elevated interleukins and chemokines, is also considered a contributing factor to vascular remodeling.
Clinical and Research Implications
The study underscores the importance of understanding sex differences in post-viral endothelial function and immune responses. Clinically, it advocates for routine cardiovascular risk assessment for patients with PACS, particularly women reporting ongoing symptoms. While CARTESIAN was not designed to test specific therapies, it emphasizes the need for aggressive management of traditional risk factors and patient education about expected recovery trajectories.
For researchers, the agenda includes validating PWV as a prognostic biomarker for PACS and exploring targeted strategies to reverse or mitigate vascular damage. Policymakers are urged to recognize the vascular legacy of COVID-19 as measurable and potentially mitigable, warranting resource allocation for longitudinal surveillance and trials to test modifiable targets.
In conclusion, the editorial paints a complex picture of COVID-19’s impact on vascular health, with women disproportionately affected. However, the potential for partial reversibility offers hope. The central challenge moving forward is to identify modifiable targets that prevent arterial stiffness during future surges and develop therapies to reduce long-term cardiovascular consequences for those already affected.