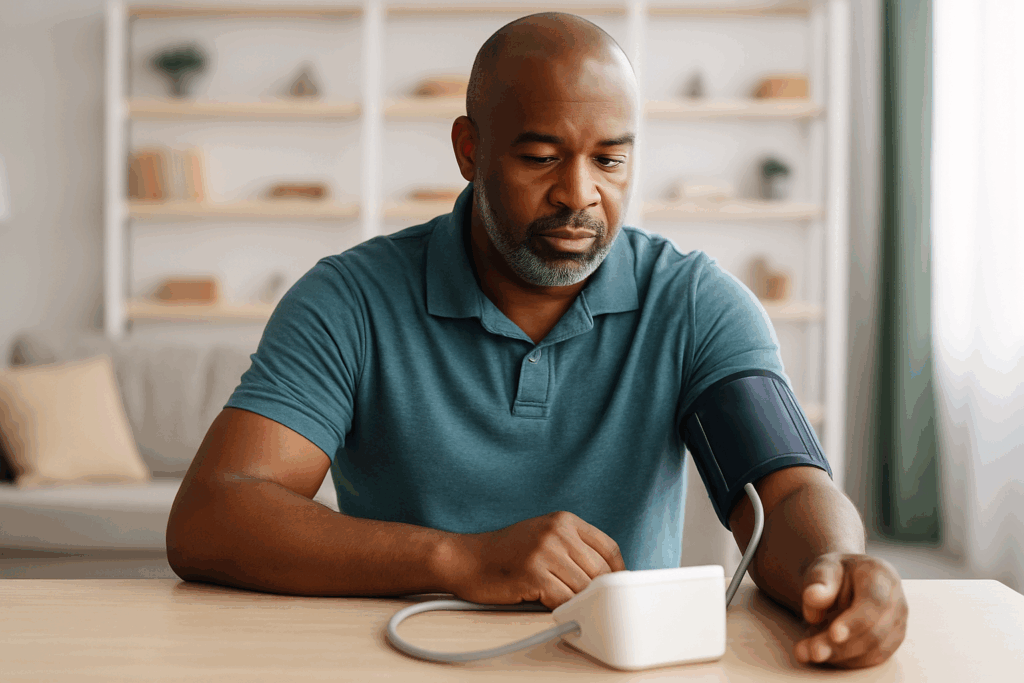
Intensive blood-pressure control, aiming for levels below 120 mm Hg, has been shown to prevent more heart-related events than traditional targets, even when accounting for real-world measurement errors. This aggressive approach is not only more protective but also cost-effective, with an estimated cost of about $42,000 per quality-adjusted life-year gained.
However, this strategy is not without its challenges. It carries added risks such as falls or kidney issues and necessitates increased medication use and clinic visits, making it unsuitable as a universal solution. High blood pressure, a significant health concern, is closely linked to heart attacks, strokes, and heart failure. Traditionally, the target has been to maintain systolic pressure under 130 or 140 mm Hg. Nevertheless, new research from Mass General Brigham suggests that aiming for a lower target—below 120 mm Hg—offers more protection and is a wise health investment.
“Our findings suggest the intensive <120 mm Hg target prevents more cardiovascular events and provides good value, and this holds true even when measurements aren’t perfect,” researcher Karen Smith, Ph.D., stated in a news release.
Understanding the Study
The research team employed a simulation model that integrated data from reputable sources such as the SPRINT clinical trial, nationwide surveys, and other published studies. They examined three blood-pressure targets: under 140, under 130, and under 120 mm Hg. The model also considered the typical measurement errors that occur in everyday clinical settings.
The simulation assessed long-term health outcomes, including heart attacks, strokes, and heart failure, while balancing these against adverse treatment events like falls, kidney damage, low blood pressure, and slow heart rate. It also factored in the increased costs associated with more medications and clinic visits.
Key Findings
Despite real-world measurement inaccuracies, targeting blood pressure below 120 mm Hg was found to prevent more cardiovascular events compared to the 130 mm Hg goal. Moreover, the cost per quality-adjusted life-year was approximately $42,000, a figure considered cost-effective in the U.S. healthcare context.
“This study should give patients at high cardiovascular risk and their clinicians more confidence in pursuing an intensive blood pressure goal,” Dr. Smith emphasized in the news release.
While the findings are promising, researchers noted that these lower blood pressure targets led to increased healthcare spending due to more frequent doctor visits and a higher risk of adverse events related to blood pressure treatment, such as falls, kidney injury, hypotension, and bradycardia.
Identifying Suitable Candidates
The researchers highlighted the importance of doctors determining which patients are the best candidates for these stricter blood pressure regulations. Dr. Smith explained, “Our results examine the cost-effectiveness of intensive treatment at the population level. However, given the additional risk of adverse events related to antihypertensives, intensive treatment will not be optimal for all patients. Patients and clinicians should work together to determine the appropriate medication intensity based on patient preferences.”
Implications and Future Directions
The study’s implications extend beyond individual patient care, potentially influencing broader public health strategies and guidelines. As healthcare providers consider these findings, they must balance the benefits of intensive blood pressure control against the potential risks and costs.
Looking ahead, further research could explore personalized approaches to blood pressure management, taking into account genetic, lifestyle, and demographic factors that may affect treatment efficacy and safety. As the medical community continues to refine its understanding of hypertension management, patients are encouraged to engage in open dialogues with their healthcare providers to make informed decisions about their treatment plans.
This development in blood pressure management represents a significant shift in how cardiovascular health is approached, emphasizing the need for tailored treatment strategies that consider the unique needs and risks of each patient.