Researchers at the University of Cambridge have uncovered why common cuff-based blood pressure readings may often be misleading and proposed methods to improve their accuracy. This revelation could significantly impact patient health outcomes, as hypertension remains the leading risk factor for premature death worldwide, linked to heart disease, strokes, and heart attacks.
Alarmingly, inaccuracies in the widely used auscultatory method of blood pressure measurement might result in up to 30% of hypertension cases being undiagnosed. The study, published in the journal PNAS Nexus, offers a new understanding of the mechanics behind these inaccuracies and suggests straightforward changes that could enhance the precision of these measurements.
Understanding the Auscultatory Method
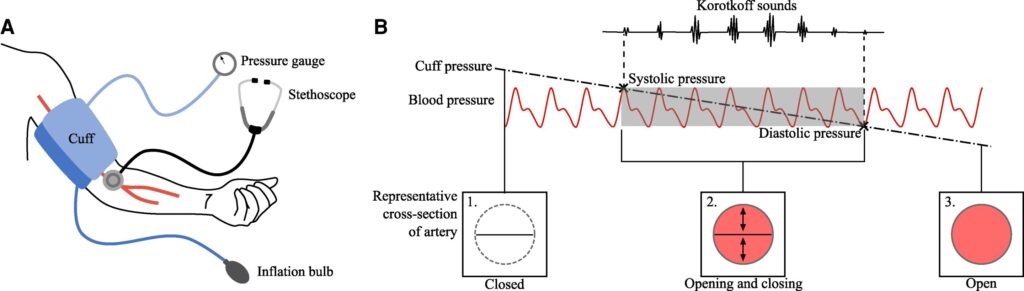
The auscultatory method, familiar to anyone who has had their blood pressure checked, involves inflating a cuff around the upper arm to cut off blood flow. A clinician then listens for tapping sounds through a stethoscope as the cuff deflates, determining blood pressure from a gauge attached to the cuff. The reading consists of two numbers: systolic (maximum) and diastolic (minimum) pressure, with 120/80 considered ideal.
Despite being the gold standard, this method has been found to overestimate diastolic pressure and underestimate systolic pressure. “We have a good understanding of why diastolic pressure is overestimated, but why systolic pressure is underestimated has been a bit of a mystery,” explained co-author Kate Bassil from Cambridge’s Department of Engineering.
Exploring the Causes of Inaccuracy
Previous studies using rubber tubes failed to replicate how arteries collapse under cuff pressure, masking the underestimation effect. The Cambridge researchers developed a simplified physical model to study the effects of downstream blood pressure—the pressure in the arm below the cuff. Their findings revealed that low downstream pressure causes the artery to remain closed longer during cuff deflation, delaying reopening and leading to underestimation.
“We are currently not adjusting for this error when diagnosing or prescribing treatments, which has been estimated to lead to as many as 30% of cases of systolic hypertension being missed,” said Bassil.
Instead of rubber tubes, the researchers used tubes that lay flat when deflated and fully closed under cuff pressure, mimicking the low downstream pressure observed in the body.
Proposed Solutions and Future Directions
To address these inaccuracies, the researchers suggest simple protocol adjustments, such as raising the arm before measurement to produce a predictable downstream pressure. This change does not require new devices, merely a modified approach. “You might not even need new devices, just changing how the measurement is done could make it more accurate,” said co-author Professor Anurag Agarwal.
Should new devices be developed, they could incorporate additional inputs like age, BMI, or tissue characteristics to adjust readings for individual patients. The researchers are seeking funding for clinical trials to test their findings in patients and are looking for partners to refine their models and validate effects across diverse populations. Collaboration with clinicians will be crucial to implement these changes in clinical practice.
Implications for Global Health
This development follows growing concerns about the accuracy of medical diagnostics and their implications for public health. Accurate blood pressure readings are vital for effective hypertension management, which can prevent severe health issues. By improving measurement accuracy, healthcare providers can better diagnose and treat patients, potentially reducing the burden of cardiovascular diseases globally.
As the research progresses, the potential for improved health outcomes becomes increasingly tangible. The move represents a significant step towards more reliable and individualized patient care, addressing a long-standing gap in medical diagnostics.