A groundbreaking study conducted by researchers from the Broad Institute of MIT and Harvard, alongside Mass General Brigham, has unveiled that continuous exposure to low-oxygen environments can protect against neurodegeneration and even restore movement in a mouse model of Parkinson’s disease (PD). Published in Nature Neuroscience, the study suggests a novel therapeutic strategy that could potentially prevent or reverse PD progression by limiting oxygen availability to the brain.
“The fact that we actually saw some reversal of neurological damage is really exciting,” said co-senior author Dr. Vamsi Mootha, an institute member at the Broad and a professor at Harvard Medical School. “It tells us that there is a window during which some neurons are dysfunctional but not yet dead—and that we can restore their function if we intervene early enough.”
Exploring Hypoxia’s Neuroprotective Potential
The current research builds on over a decade of findings by Mootha and his colleagues into hypoxia, a condition characterized by lower-than-normal oxygen levels in the body and its tissues. Anecdotal evidence from PD patients suggests symptom improvement at high altitudes, and studies have linked heavy smoking, which reduces oxygen delivery due to elevated carbon monoxide, to a lower risk of PD.
Research into other rare neurodegenerative disorders, such as Leigh syndrome and Friedreich’s ataxia, has also highlighted hypoxia’s protective role against mitochondrial disruptions that cause these diseases. “Based on this evidence, we became very interested in the effect of hypoxia on Parkinson’s disease,” said co-senior author Dr. Fumito Ichinose, a professor of anesthesia at Harvard Medical School and MGH.
Methodology and Findings
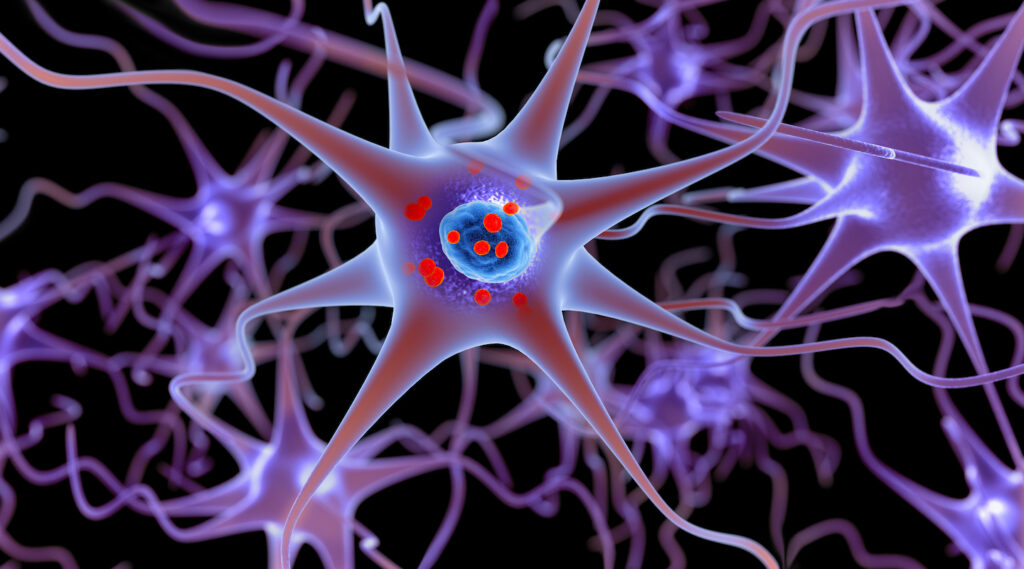
To investigate hypoxia’s effects, the team employed a well-established mouse model of PD. Mice were injected with preformed fibrils (PFFs) of α-synuclein, leading to the aggregation of Lewy bodies and subsequent neurodegeneration of dopamine-producing neurons in the substantia nigra pars compacta (SNpc). One group of mice was kept in normal oxygen conditions (21%), while another group was housed in continuous low-oxygen conditions (11%), akin to high-altitude environments around 4,800 meters.
Data from the experiment revealed that mice breathing normal air developed high levels of Lewy bodies, experienced significant loss of dopaminergic neurons, and suffered severe motor dysfunction. In contrast, mice exposed to low-oxygen conditions from the onset did not lose neurons and showed no signs of movement impairment.
“These results suggest that hypoxia may have neuroprotective effects downstream of α-syn aggregation in PD, even after symptom onset and neuropathological changes,” the researchers wrote.
Understanding the Mechanisms
The study further explored the effects of a low-oxygen environment on mice already exhibiting PD symptoms and neuron loss, introducing them to hypoxia six weeks post-PFF injection. In these cases, the progression of neurodegeneration halted, motor skills improved, and anxiety-like behaviors diminished.
Interestingly, hypoxia did not prevent α-syn aggregation but appeared to shield neurons from the toxic effects of these aggregates. Tissue analysis showed that mice with PD-like symptoms under normal oxygen conditions had excess oxygen levels in brain regions, consistent with mitochondrial dysfunction and impaired oxygen utilization. Damaged mitochondria fail to efficiently consume oxygen, resulting in tissue hyperoxia.
“Too much oxygen in the brain turns out to be toxic,” said Mootha. “By reducing the overall oxygen supply, we’re cutting off the fuel for that damage.”
Potential Pathways and Future Directions
The researchers propose that reducing oxygen levels may protect neurons by both directly lowering tissue hyperoxia and indirectly activating hypoxia-inducible factor (HIF)-dependent pathways, which reduce lipid peroxidation and protect mitochondrial function. RNA sequencing and proteomic analysis of substantia nigra tissue revealed strong upregulation of HIF target genes in low-oxygen-treated mice.
“Our data support the notion that both HIF-dependent and HIF-independent mechanisms may be at play in conferring the observed neuroprotection,” the researchers wrote.
Challenges and Future Implications
The team acknowledged the study’s limitations, noting that analyses were conducted on the entire substantia nigra region rather than isolating the SNpc and its dopaminergic neurons. They also emphasized the need for longer follow-up studies to examine additional pathological changes and assess effects in aging models.
Currently, the findings are not directly translatable to human patients, and the investigators strongly discourage unsupervised exposure to low-oxygen environments, as unsupervised or intermittent hypoxia can be dangerous and might worsen the disease. However, efforts are underway to develop “hypoxia in a pill” drugs, targeted at other mitochondrial disorders, which mimic the neuroprotective effects of low-oxygen exposure without the associated risks.
“It may not be a treatment for all types of neurodegeneration,” Mootha said, “but it’s a powerful concept—one that might shift how we think about treating some of these diseases.”