A groundbreaking development in wearable technology could significantly improve the management of bipolar disorder by allowing patients to monitor their lithium levels through sweat. This innovative sensor, developed by researchers at the University of Southern California (USC), promises a non-invasive, convenient alternative to traditional blood tests.
Lithium remains a cornerstone in the treatment of bipolar disorder due to its efficacy. However, it carries a narrow therapeutic window, where doses that are too high can lead to severe side effects, including kidney and thyroid damage, or even death. Conversely, insufficient doses render the treatment ineffective. Regular monitoring of lithium levels is crucial, but current methods are cumbersome and invasive, requiring blood draws that are often inconvenient and painful.
Revolutionizing Lithium Monitoring
The new wearable sensor aims to simplify this process, as explained by Yasser Khan, a professor at USC’s Ming Hsieh Department of Electrical and Computer Engineering. “Our goal was to create an easy-to-use sensor that bypasses the need for blood draws entirely,” said Khan, who leads the USC Khan Lab and is part of the USC Institute for Technology and Medical Systems.
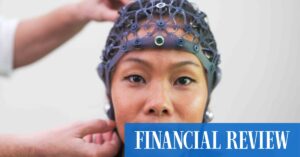
The study, published in the journal Device, highlights the sensor’s ability to use sweat as an alternative to blood samples. Sweat can be collected non-invasively and reflects lithium concentrations in real time. The wearable device includes a skin-safe, iontophoresis-based system that induces sweat without physical exertion, transmitting data directly to a smartphone app for patient convenience.
Innovative Technology Behind the Sensor
The sensor’s core innovation lies in its use of organic electrochemical transistors (OECTs), which are designed specifically for lithium detection. These devices convert ionic signals in liquid into readable electronic data. Unlike conventional OECTs, which involve complex fabrication, the USC-developed sensor uses a novel material formulation tailored for lithium ions, allowing for a fully printed and scalable production process.
“We developed the entire lithium monitoring system—from the OECT-based sensor patch and on-demand sweat induction to the readout electronics and smartphone app—using a simple, scalable, and cost-effective fabrication process,” said Mohammad Shafiqul Islam, the study’s first author and a Ph.D. student in the Khan Lab.
Clinical Testing and Patient Feedback
The sensor has already moved beyond the lab, with testing conducted in collaboration with psychiatrist Adam Frank, MD, Ph.D., at the Keck School of Medicine. During pilot trials, patients using the wearable device provided sweat samples, which were successfully matched against results from traditional commercial sensors. The feedback was overwhelmingly positive, with patients expressing relief at the prospect of monitoring their health without frequent hospital visits.
“The ability to noninvasively monitor lithium levels will improve care for patients taking lithium, who typically require regular blood draws to assess lithium levels,” said Frank. “Being able to track these levels continuously over time will improve safety by allowing for medication dose adjustments that avoid side effects and potential medication toxicity.”
Looking Ahead: AI Integration and Broader Implications
The research team is now focusing on further advancements, including the integration of artificial intelligence to automatically adjust lithium dosages for optimal therapeutic benefits without risking toxicity. This development could represent a significant leap forward in personalized medicine, offering a model for other chronic conditions requiring precise medication management.
The implications of this innovation extend beyond individual patient care. By enabling more frequent and accurate monitoring, the sensor could reduce healthcare costs associated with emergency interventions due to incorrect dosing. Furthermore, it underscores the growing role of wearable technology in transforming healthcare delivery, potentially setting a precedent for future developments in the field.
As the team continues to refine the technology, the hope is that this sensor will soon become a standard tool in the management of bipolar disorder, providing patients with greater autonomy and peace of mind in their treatment journey.