Melbourne scientists have made significant strides in understanding the “Hippo pathway” at the molecular level, unveiling its potential as a crucial target for treating mesothelioma, a deadly form of cancer. This groundbreaking research, conducted at the Peter MacCallum Cancer Centre, has captured the first-ever microscopy footage showing the activity of DNA-binding proteins known as TEADs and YAP, which are essential to the Hippo pathway’s function.
Professor Kieran Harvey, a leading researcher in the study, explains that the Hippo pathway originated over a billion years ago and remains consistent across a wide range of species, from single-celled organisms to humans. It plays a vital role in regulating tissue and organ growth, wound healing, and cell proliferation and death. The pathway’s malfunction is linked to cancer development, making it a prime target for new therapeutic strategies.
New Drugs Undergoing Trials
Currently, two new drugs targeting the Hippo pathway are in the early stages of human trials at Peter Mac, being evaluated for their efficacy in treating mesothelioma. This cancer is notoriously difficult to treat and is often caused by asbestos exposure. Professor Harvey, who holds positions at both Peter Mac and Monash University, highlights the significance of these trials.
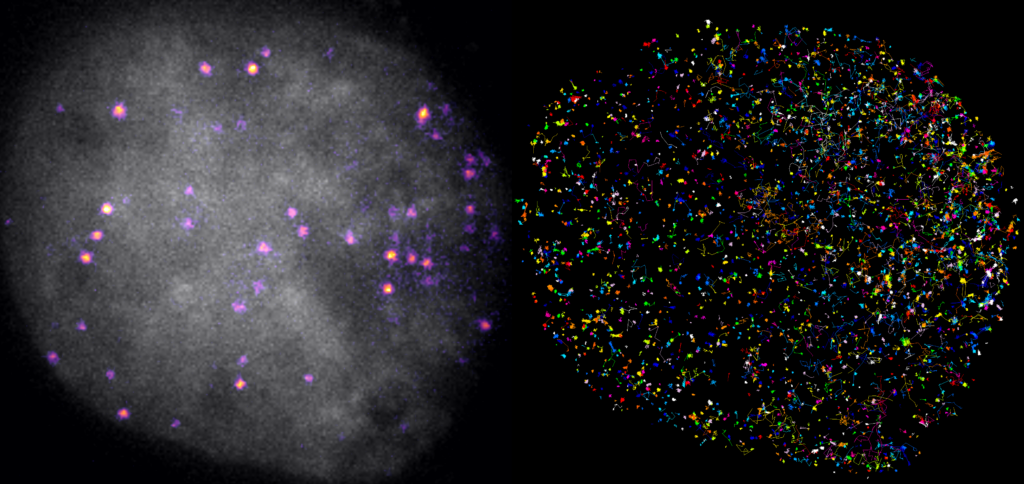
“The Hippo pathway controls transcription, which is how the body carries out the instructions from our DNA, but how it does this is poorly understood,” says Professor Harvey. “In this study, we used new microscopy techniques that allowed us to record – for the first time ever – how proteins involved in this signaling pathway work in real time.”
Understanding Protein Interactions
The research team, including Dr. Benjamin Kroeger, utilized advanced microscopy to observe how proteins interact with DNA over varying timescales. A key discovery is that the Hippo pathway influences gene expression by controlling the duration that TEADs and YAP bind to DNA. This finding is particularly relevant for mesothelioma, as TEAD1, one of the TEAD proteins, is implicated in the cancer’s development and progression.
Furthermore, the study revealed that a mutated version of YAP, known as YAP-TFE3, binds to DNA for longer periods than its unmutated counterparts. This mutation is associated with another rare cancer, epithelioid hemangioendothelioma, underscoring the broader implications of the research.
Implications for Cancer Treatment
The research, recently published in the journal Science Advances, offers promising insights into how these proteins could be targeted by new cancer drugs. The study’s findings pave the way for potential breakthroughs in treating mesothelioma and other hard-to-treat cancers.
“Given its foundational role, we hold great hopes that improving understanding of how the Hippo pathway works will open new avenues for treating mesothelioma and other hard-to-treat cancers,” Professor Harvey states.
Future Directions
The ongoing trials and research efforts at institutions like Peter Mac and Monash University underscore the importance of continued exploration into the Hippo pathway. As scientists deepen their understanding of this ancient biological mechanism, the potential for developing effective cancer treatments grows.
For more information, the Peter Mac Communications team can be contacted at 0417 123 048, or Cheryl Critchley at Monash University at 0477 571 442 or [email protected] Microscopy videos and related images are available for media use and can be downloaded from a provided Dropbox link.
Peter MacCallum Cancer Centre is a world-leading cancer research, education, and treatment center, dedicated to caring for individuals affected by cancer. Monash University, with over 60 years of research excellence, continues to address global challenges through its Impact 2030 strategic plan.






