A recent study published in BMJ Mental Health has unveiled significant concerns regarding the prescription of antipsychotic treatments to children and young people (CYP). The research highlights inappropriate prescribing practices and insufficient aftercare monitoring by general practitioners (GPs), raising alarms about the clarity of best practice guidelines and the completeness of data available to researchers.
The study, led by Dr. Yana Vinogradova from the University of Nottingham’s School of Medicine, suggests that inconsistencies in NICE (National Institute for Health and Care Excellence) guidelines across different treatment settings, alongside gaps in anonymized patient data, contribute to these issues.
Antipsychotics and Their Impact on Young People
Antipsychotics, known for their severe physical side effects, particularly affect children and adolescents. NICE has developed comprehensive guidelines for prescribing and aftercare for conditions like psychosis and bipolar disorder, recommending that secondary care specialists handle initial prescriptions and health monitoring for at least 12 months before transferring care to GPs under “shared care” arrangements.
While antipsychotics are not recommended as core treatments for conditions such as autism or Tourette’s syndrome, NICE guidelines do allow for short-term, off-label use for severe symptoms. However, the guidance on prescribing and aftercare for these conditions remains rudimentary, lacking references to more detailed best practice guidelines.
Inappropriate Use and Rising Concerns
Concerns about the inappropriate use of antipsychotics to manage “challenging behavior” in CYP have led to initiatives like the NHS-supported project launched in 2018, aiming to reduce such prescriptions. The new study focused on four mental health conditions linked to antipsychotic treatment in NICE guidelines, using encoded English general practice data.
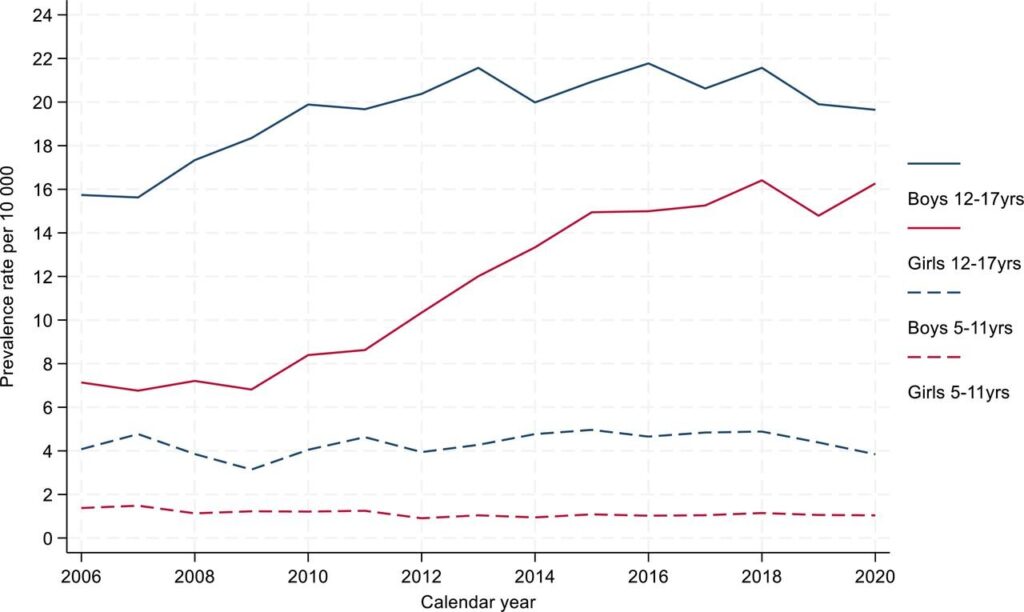
The study aimed to describe trends in antipsychotic prescribing, reasons for prescriptions, treatment lengths, and compare health monitoring levels between CYP with and without antipsychotic prescriptions. Dr. Vinogradova noted an increase in antipsychotic prescriptions from 2006 to 2021, particularly among adolescent females.
“Our findings showed rises in levels of antipsychotics prescribing to CYP between 2006 and 2021—greater in adolescence than in childhood and greatest among adolescent females,” Dr. Vinogradova stated.
Alarmingly, only just under half of the prescriptions were for the focus mental health conditions, with 62% associated with autism. Some prescriptions were linked to conditions like ADHD, learning difficulties, and self-harm, raising questions about adherence to NICE guidelines.
Challenges in Data and Monitoring
Dr. Vinogradova expressed concerns about the low levels of health monitoring, especially for conditions like autism and Tourette’s, compared to psychosis or bipolar disorder. The study found more records for basic health measurements than laboratory tests, indicating a gap in comprehensive monitoring.
“Taken at face value, these findings appear to be disturbing evidence of lack of adherence to NICE guidelines,” Dr. Vinogradova remarked, emphasizing the need for more complete data to accurately audit adherence to best practices.
The study calls for streamlined, centralized best practice recommendations for antipsychotic treatments, covering both core and off-label uses, to improve adherence across treatment environments. The separation of primary and secondary care records, with secondary care information often transferred in text form, contributes to data incompleteness.
Looking Forward: The Need for Comprehensive Data
Dr. Vinogradova highlighted the need for studies with access to more complete data to establish reliable estimates of adherence to best practices. The current separation of care records and varying data flows complicate the process, necessitating a different research approach to ensure data completeness and accuracy.
The study underscores the importance of addressing these challenges to optimize antipsychotic treatment practices for CYP, ensuring adherence to guidelines and improving health outcomes. As the healthcare community moves forward, efforts to streamline data collection and enhance guideline clarity will be crucial in safeguarding the well-being of young patients.







