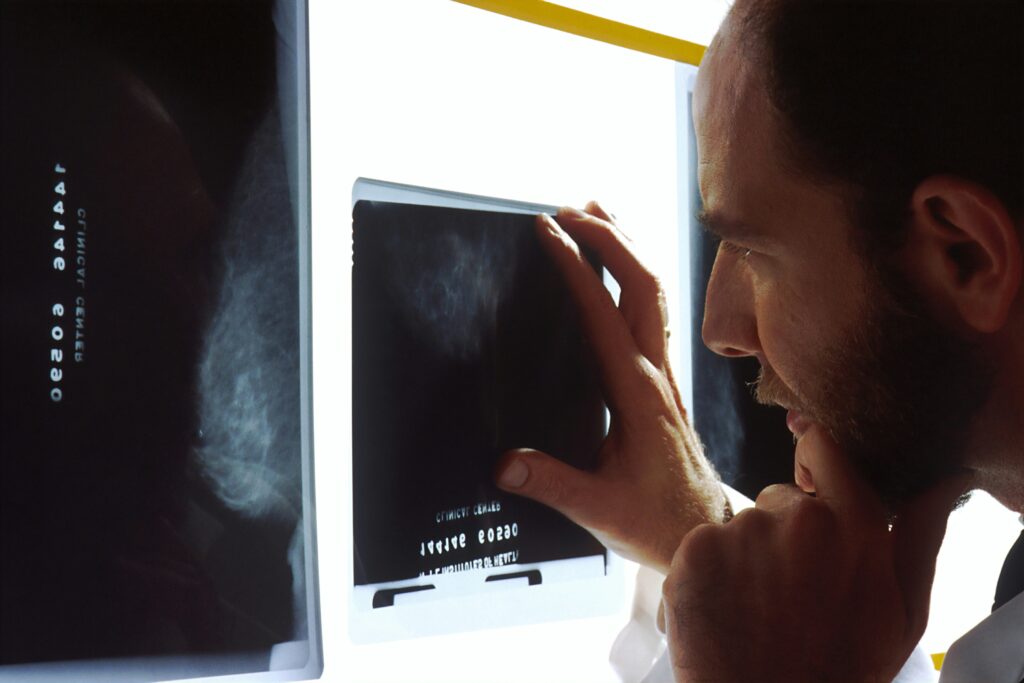
SAN FRANCISCO—In a revelation that could influence the dietary guidelines for patients on anti-obesity medications, a recent study presented at ENDO 2025, the Endocrine Society’s annual meeting in San Francisco, highlights the potential of higher protein intake to mitigate muscle loss in women and older adults taking semaglutide.
The study underscores a critical concern in the treatment of obesity: the loss of muscle mass, or lean mass, which often accompanies weight reduction. This phenomenon can adversely impact metabolism and bone health, as muscle plays a vital role in regulating blood sugar post meals and maintaining bone strength, according to Dr. Melanie Haines, the study’s lead researcher from Massachusetts General Hospital and Harvard Medical School.
Understanding the Impact of Semaglutide
Semaglutide, a GLP-1 receptor agonist, has gained attention for its efficacy in promoting weight loss. However, approximately 40% of the weight lost through this medication is attributed to lean mass, including muscle. Dr. Haines notes that the specific demographics most susceptible to muscle loss and the subsequent effects on blood sugar levels remain unclear.
The study involved 40 adults with obesity over a three-month period. Of these, 23 participants were prescribed semaglutide, while 17 adhered to a diet and lifestyle program named Healthy Habits for Life (HHL). The research aimed to assess changes in muscle mass among the participants.
Comparative Analysis of Weight Loss Methods
Findings revealed that those on semaglutide experienced greater overall weight loss compared to the HHL group. However, the proportion of weight loss attributed to lean mass was similar across both groups. This highlights a crucial insight: the type of weight loss intervention does not necessarily alter the proportion of muscle loss.
Further analysis indicated that within the semaglutide group, older adults, females, and those with lower protein intake were more prone to muscle loss. Additionally, a greater degree of muscle loss was associated with a less significant improvement in blood sugar levels, as measured by HbA1c.
“Older adults and women may be more likely to lose muscle on semaglutide, but eating more protein may help protect against this,” Dr. Haines emphasized. “Losing too much muscle may reduce the benefits of semaglutide on blood sugar control. This means preserving muscle during weight loss with semaglutide may be important to reduce insulin resistance and prevent frailty in people with obesity.”
Implications for Future Treatment Strategies
The findings of this study suggest a potential modification in dietary recommendations for patients undergoing treatment with semaglutide. Increasing protein intake could be a viable strategy to preserve muscle mass, thereby enhancing the overall benefits of the medication.
Dr. Haines advocates for further research to determine the optimal balance between fat loss and muscle preservation when utilizing GLP-1 medications. This could pave the way for more personalized and effective obesity treatment plans, particularly for vulnerable populations such as older adults and women.
Broader Context and Historical Perspectives
The concern over muscle loss in weight loss programs is not new. Historically, the focus has often been on the numbers on the scale, sometimes at the expense of muscle health. This study adds to a growing body of evidence that suggests a more nuanced approach is necessary—one that considers both the quantity and quality of weight loss.
The announcement comes as healthcare providers increasingly recognize the importance of muscle health in managing obesity and related conditions. The potential to tailor dietary interventions based on individual risk factors could revolutionize how obesity is treated, particularly in an aging population.
Looking Ahead
As the medical community continues to explore the complexities of weight loss and its impact on overall health, studies like this underscore the need for comprehensive treatment strategies. The integration of dietary adjustments, such as increased protein intake, could be a key component in maximizing the benefits of medications like semaglutide.
Future research will likely focus on identifying specific protein intake levels that can effectively counteract muscle loss while still achieving significant fat reduction. This could lead to more refined guidelines that help patients achieve healthier, more sustainable weight loss outcomes.
In conclusion, while semaglutide remains a powerful tool in the fight against obesity, its use must be carefully managed to ensure that patients do not compromise their muscle health in the process. The insights from this study provide a promising avenue for enhancing the efficacy and safety of obesity treatments.