Researchers at the Johns Hopkins Kimmel Cancer Center and the Bloomberg~Kimmel Institute for Cancer Immunotherapy have unveiled updated guidelines to standardize how pathologists assess tumor response to neoadjuvant therapy across various solid tumor types. These guidelines, supported by a reproducibility study, aim to create a unified framework for evaluating the effects of presurgical treatments.
The initiative, partly funded by the National Institutes of Health and The Mark Foundation, was developed in collaboration with the Society for Immunotherapy of Cancer (SITC) and the International Neoadjuvant Melanoma Consortium (INMC). The recommendations, published in the Annals of Oncology on November 4, provide a comprehensive framework for assessing residual viable tumor (RVT), necrosis, and regression after neoadjuvant therapy.
Background and Development of the Guidelines
The updated guidelines refine earlier criteria proposed for lung cancer in 2018 and expanded in 2020 to a pan-tumor approach. These revisions are based on five years of real-world application, field inquiries, and new reproducibility data. A related study, published earlier this year, confirmed the guidelines’ applicability across different tumor types, achieving consistent results globally.
Lead author Dr. Julie Stein Deutsch emphasized the importance of a unified scoring system, stating, “Neoadjuvant therapy is rapidly expanding across cancer types, and pathologic response is emerging as a predictor of long-term survival and an important clinical trial endpoint.” She noted that previous scoring systems varied widely, complicating cross-study comparisons and practical applications.
Significance of a Unified Approach
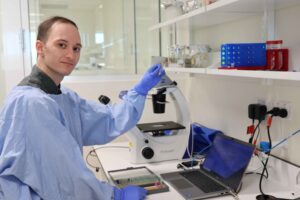
The guidelines were prompted by evidence showing consistent tissue changes across cancer types when viewed under a microscope, especially following immunotherapy. The research team analyzed approximately 500 specimens treated with anti-PD-1 immunotherapy, observing similar response patterns regardless of tumor origin.
Dr. Janis Taube, senior author and director of dermatopathology at Johns Hopkins, highlighted the inefficiency of switching between multiple scoring systems. “Most pathologists around the world are generalists, not tumor-type specialists,” she explained. The unified system aims to streamline processes and improve reporting consistency.
Reproducibility and Future Implications
A major advancement of the new guidelines is their demonstrated reproducibility. An international study involving 14 pathologists showed high concordance in scoring RVT, regression, and necrosis using the updated criteria. These findings were presented at the American Society of Clinical Oncology annual meeting in 2024, reinforcing the rationale for a pan-tumor approach.
Dr. Deutsch stressed the importance of reproducibility, stating, “Different pathologists must arrive at similar scores if these metrics are going to guide patient care and clinical trials.” The team is collaborating with SITC to distribute training materials and resources to ensure widespread adoption.
Next Steps and Research Support
Future efforts will focus on refining RVT thresholds specific to tumor types as more survival data becomes available. The research was supported by numerous organizations, including The Mark Foundation for Cancer Research, the Bloomberg~Kimmel Institute, and the National Institutes of Health.
Contributors to the study include a diverse group of researchers from various institutions, reflecting a broad collaborative effort. The terms of their consulting and funding arrangements are managed by Johns Hopkins University in accordance with its conflict-of-interest policies.
The updated guidelines represent a significant step forward in standardizing tumor response assessment, promising to enhance clinical care, research, and regulatory processes across the oncology field.