Chronic wounds, particularly prevalent among individuals with diabetes, pose a significant health challenge, often leading to lower-limb amputations. These wounds are exacerbated by persistent infections that hinder the healing process. A recent study conducted by researchers from the University of Geneva (UNIGE) and Nanyang Technological University (NTU) has shed light on a novel approach to tackling this issue by targeting the bacterium Enterococcus faecalis, which actively disrupts tissue repair.
The study, jointly led by Guillaume Thibault, associate professor at NTU’s School of Biological Sciences, and Kimberly Kline, full professor in the Department of Microbiology and Molecular Medicine at UNIGE, reveals that rather than relying on antibiotics, which can promote resistance, neutralizing the harmful byproducts of E. faecalis can restore skin cell regeneration. This discovery could significantly reduce the risk of complications and amputations.
The Mechanism Behind E. faecalis
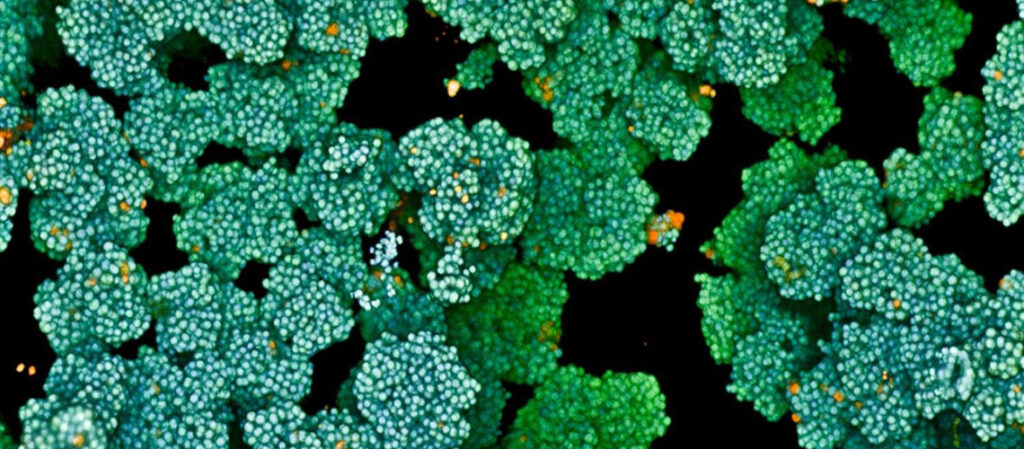
Enterococcus faecalis, a widespread opportunistic bacterium, has been found to interfere with the healing process not through a conventional toxin, but by hijacking a product of its own metabolism. According to Aaron Tan, a researcher at the Singapore Centre for Environmental Life Sciences and Engineering (SCELSE) and first author of the study, the bacterium employs a previously unrecognized metabolic process known as extracellular electron transport (EET). This process continuously produces hydrogen peroxide, a highly reactive oxygen species that can damage living tissue.
“E. faecalis uses a previously unrecognised metabolic process known as extracellular electron transport (EET), which continuously produces hydrogen peroxide, a highly reactive oxygen species that can damage living tissue,” explains Aaron Tan.
Oxidative Stress and Its Impact
Hydrogen peroxide, commonly known as an industrial disinfectant and bleaching agent, becomes problematic when generated directly within an infected wound. The researchers demonstrated that this compound induces significant oxidative stress in keratinocytes—the skin cells responsible for tissue repair. This stress activates a cellular defense mechanism linked to misfolded proteins, ultimately paralyzing the cells and preventing them from migrating to close the wound.
Neutralizing Hydrogen Peroxide
To validate the central role of this process, the scientists used a genetically modified strain of E. faecalis lacking the EET pathway. This modification led to a sharp decline in hydrogen peroxide production, allowing the bacterium to no longer impede wound healing. The team further explored whether neutralizing hydrogen peroxide could reverse the damage. By treating skin cells with catalase—a naturally occurring antioxidant enzyme that breaks down hydrogen peroxide—they reduced cellular stress and restored the cells’ ability to migrate and repair tissue.
“Our results show that the bacterium’s own metabolism is its weapon—a surprising and previously unknown discovery,” notes associate professor Thibault.
Implications for Future Treatments
This breakthrough establishes a direct link between bacterial metabolism and host cell dysfunction, paving the way for new therapeutic strategies for chronic wounds. The study suggests that wound dressings enriched with antioxidants such as catalase could represent a promising approach. In the long term, these findings may lead to new treatments for patients suffering from non-healing wounds—a major public health concern.
The announcement comes as healthcare systems worldwide grapple with the growing challenge of antibiotic resistance. By focusing on neutralizing harmful bacterial byproducts rather than eliminating the bacteria themselves, this research offers a novel and potentially more sustainable solution to a persistent problem.
As the medical community continues to seek effective treatments for chronic wounds, this study highlights the importance of understanding bacterial metabolism and its impact on human health. With further research and development, these findings could transform the management of chronic wounds, offering hope to millions of patients globally.