DALLAS, Jan. 29, 2026 — A recent study presented at the American Stroke Association’s International Stroke Conference 2026 reveals that individuals with a dissecting aneurysm associated with a cervical artery dissection (CeAD) do not face an increased risk of stroke within the first six months post-diagnosis. This finding could significantly impact how healthcare professionals approach the diagnosis and treatment of this condition.
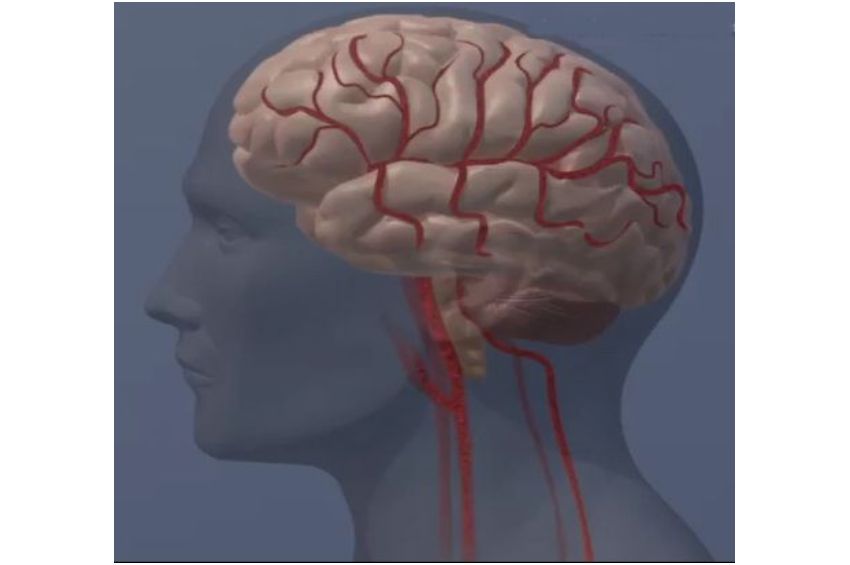
The study, which will be discussed in detail at the conference in New Orleans from February 4-6, 2026, is part of an ongoing effort to understand the implications of CeAD, a condition responsible for approximately 2% of ischemic strokes overall and up to 25% in adults under 50. CeAD occurs when a tear in the inner artery wall of the neck allows blood to leak, potentially forming a clot that could lead to a stroke. In some instances, this leads to the formation of a dissecting aneurysm, a bulge in the artery wall.
Understanding Cervical Artery Dissection and Aneurysms
Cervical artery dissection is a known cause of stroke, especially among younger adults. The new analysis, derived from the Antithrombotics for Stroke Prevention in Cervical Artery Dissection (STOP-CAD) study, offers fresh insights into the condition. Researchers conducted a secondary analysis of data from this multicenter, international study to evaluate the presence and impact of dissecting aneurysms in CeAD patients.
According to Dr. Muhib Khan, an associate professor in neurology at the Mayo Clinic, “We leveraged a large dataset from a global registry to provide a comprehensive overview of dissecting aneurysm diagnosis, monitoring, and outcomes.” The study found that dissecting aneurysms are relatively common but not life-threatening in the short term, with about 19% of the 4,000 participants developing the condition.
Key Findings and Implications
One of the significant revelations from the study is that having a dissecting aneurysm does not increase the risk of stroke compared to those with CeAD but without aneurysms. Additionally, about 10% of those with a dissecting aneurysm experienced growth in the aneurysm over six months, yet this did not correlate with a higher stroke risk.
“Reassuringly, dissecting aneurysm formation was not related to hemorrhagic stroke or increased mortality either,” said study co-author Dr. Zafer Keser from the Mayo Clinic.
This information could reshape clinical practices. Dr. Louise D. McCullough, a former chair of the International Stroke Conference, noted, “These results will probably give us a little bit of pause if we’re thinking about doing an intervention such as placing a carotid stent — which would require chronic antiplatelets — if we know the risk of recurrent strokes in patients with dissecting aneurysms is low.”
Study Design and Demographics
The STOP-CAD study included 4,008 adults with an average age of 46, equally split between men and women. Participants were predominantly white (73.5%), with Hispanic (9.2%), Black (6%), and Asian (3.7%) individuals also represented. The study spanned 63 sites across 16 countries, coordinated by the Department of Neurology at the Warren Alpert Medical School of Brown University.
Data on clinical, imaging, management, and outcomes were collected centrally for six months following the initial CeAD presentation. While the study provides valuable insights, researchers acknowledge its limitations, including the retrospective design and reliance on image reviews by radiologists and neurologists without a standardized process.
Looking Ahead
The findings from this study are considered preliminary until published in a peer-reviewed journal. However, they offer a promising direction for future research and clinical practice. A year-long study with a prospective design could further validate these results and refine treatment protocols.
As the medical community continues to explore the nuances of CeAD and dissecting aneurysms, this study represents a step forward in understanding and managing these complex conditions. The insights gained could lead to more tailored and less invasive approaches to patient care, ultimately improving outcomes for those affected by cervical artery dissections.





