In a groundbreaking development, researchers at the University of British Columbia (UBC) have successfully demonstrated a reliable method to produce helper T cells from stem cells in a controlled laboratory environment. This advancement, published today in the journal Cell Stem Cell, addresses a significant barrier in the field of cell therapy, potentially paving the way for more accessible and cost-effective treatments for various conditions, including cancer, infectious diseases, and autoimmune disorders.
The discovery marks a pivotal moment in the evolution of engineered cell therapies, which have been transforming modern medicine. By showcasing a scalable method to cultivate multiple immune cell types, the UBC team has taken a crucial step towards making these lifesaving treatments more widely available.
The Promise and Challenge of Living Drugs
In recent years, engineered cell therapies, such as CAR-T treatments for cancer, have delivered remarkable results for patients with otherwise untreatable diseases. These therapies involve reprogramming human immune cells to recognize and attack illnesses, effectively turning them into ‘living drugs’. However, the complexity and cost of production have limited their accessibility.
Most current treatments rely on a patient’s own immune cells, necessitating weeks of customized manufacturing. According to Dr. Megan Levings, co-senior author and professor of surgery and biomedical engineering at UBC, “The long-term goal is to have off-the-shelf cell therapies that are manufactured ahead of time and on a larger scale from a renewable source like stem cells. This would make treatments much more cost-effective and ready when patients need them.”
The Role of Helper T Cells
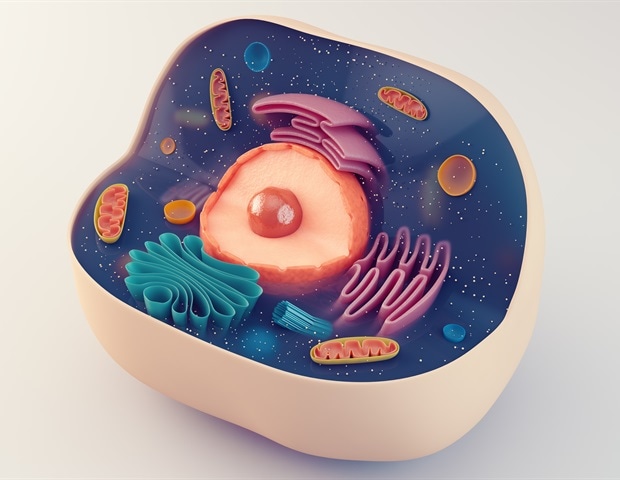
For cell therapies to be most effective, both killer T cells and helper T cells are needed. Killer T cells directly attack infected or cancerous cells, while helper T cells act as conductors of the immune system, detecting health threats, activating other immune cells, and sustaining immune responses over time. Although progress has been made in generating killer T cells from stem cells, reliably producing helper T cells has remained elusive.
“Helper T cells are essential for a strong and lasting immune response,” said Dr. Levings. “It’s critical that we have both to maximize the efficacy and flexibility of off-the-shelf therapies.”
A Major Step Toward Stem Cell-Grown Therapies
The UBC researchers have now overcome this challenge by adjusting key biological signals during cell development to precisely control whether stem cells develop into helper or killer T cells. A developmental signal known as Notch plays a critical role in this process. While Notch is necessary early in immune cell development, prolonged activity prevents the formation of helper T cells.
“By precisely tuning when and how much this signal is reduced, we were able to direct stem cells to become either helper or killer T cells,” explained Dr. Ross Jones, co-first author and research associate in the Zandstra Lab. “We were able to do this in controlled laboratory conditions that are directly applicable in real-world biomanufacturing, which is an essential step toward turning this discovery into a viable therapy.”
Real-World Implications
Importantly, the lab-grown helper T cells not only resembled real immune cells but also behaved like them. They displayed markers of healthy mature cells, carried a diverse range of immune receptors, and could specialize into subtypes that play distinct roles in immunity.
“These cells look and act like genuine human helper T cells,” said co-first author Kevin Salim, a UBC PhD student in the Levings Lab. “That’s critical for future therapeutic potential.”
The ability to generate both helper and killer T cells—and to control the balance between them—will significantly enhance the efficacy of stem cell-grown immune therapies moving forward.
Future Prospects and Clinical Applications
Dr. Peter Zandstra, co-senior author and director of the UBC School of Biomedical Engineering, emphasized the impact of this breakthrough: “This is a major step forward in our ability to develop scalable and affordable immune cell therapies. This technology now forms the foundation for testing the role of helper T cells in supporting the elimination of cancer cells and generating new types of helper T cell-derived cells, such as regulatory T cells, for clinical applications.”
As the field of cell therapy continues to evolve, this discovery represents a significant advancement toward making these treatments more accessible and effective. The research team’s work lays the groundwork for future studies and potential clinical trials, offering hope for patients worldwide who may benefit from these innovative therapies.







