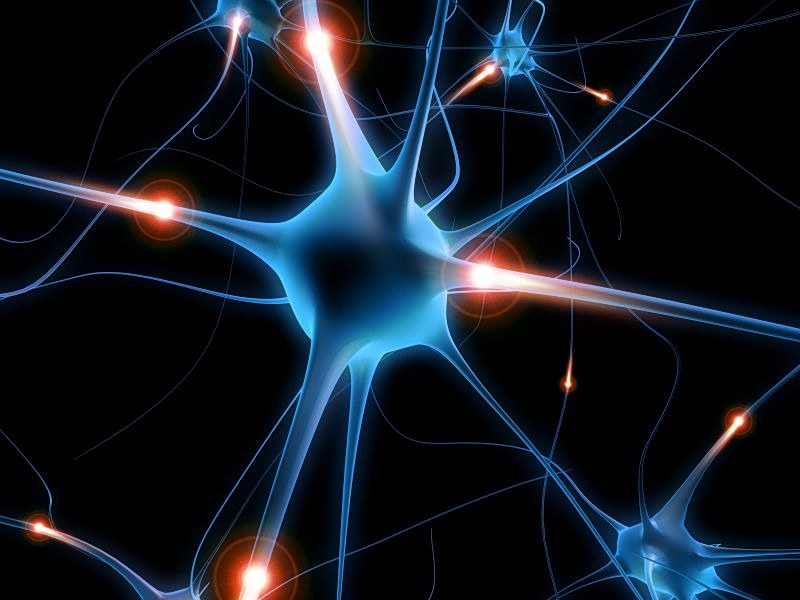
A groundbreaking study from South Korea has revealed that a bacterium commonly associated with tooth decay may also play a role in the development of Parkinson’s disease. This discovery, published in Nature Communications, offers new insights into the possible causes of this neurodegenerative disorder.
Researchers from Seoul National University College of Medicine, Pohang University of Science and Technology, and Sungkyunkwan University have identified that Streptococcus mutans, when colonizing the gut, can produce substances that enter the bloodstream and reach the brain, potentially damaging neurons responsible for movement.
How the Bacterium Affects the Brain
The study highlights that S. mutans produces an enzyme called UrdA and a metabolic byproduct known as ImP (imidazole propionate). Elevated levels of these compounds were found in the intestines and blood of individuals with Parkinson’s disease. ImP, in particular, was shown to travel to the brain, where it contributes to the degradation of dopamine-producing neurons and triggers inflammation.
Experiments conducted on mice reinforced these findings. When S. mutans was introduced into the gut or when E. coli was engineered to produce UrdA, there was a significant increase in ImP levels in both the blood and brain. The mice subsequently exhibited hallmark symptoms of Parkinson’s: neuronal damage, brain inflammation, motor difficulties, and an accumulation of α-synuclein, a protein associated with the progression of the disease.
“The presence of these compounds in the brain leads to the activation of a protein complex called mTORC1, which is crucial in the development of Parkinson’s symptoms,” the study notes.
Further experiments demonstrated that mice treated with an mTORC1 inhibitor showed reduced brain inflammation, less neuronal loss, decreased α-synuclein buildup, and improved motor function.
Implications for Treatment and Prevention
The findings underscore the importance of the mouth-gut-brain axis in understanding and potentially mitigating Parkinson’s disease. Maintaining oral hygiene and gut health could not only protect against dental and digestive issues but also reduce the risk of neurodegeneration.
According to experts, future therapies that focus on the gut and oral microbiota may offer promising new approaches for preventing or slowing the progression of Parkinson’s disease. This could represent a significant shift in how the medical community approaches the treatment of neurodegenerative disorders.
Expert Opinions and Historical Context
Dr. Lee Chang-min, a neurologist not involved in the study, commented, “This research opens up a new frontier in our understanding of Parkinson’s disease. It highlights the intricate connections between different bodily systems and how they can impact brain health.”
Historically, Parkinson’s disease has been attributed to genetic factors and environmental influences. However, this study adds a new dimension by suggesting that microbial activity in the gut could be a critical factor. The idea that bacteria in the mouth and gut could influence brain health is not entirely new, but this research provides concrete evidence linking specific bacteria to Parkinson’s symptoms.
Looking Forward
The announcement comes as the scientific community increasingly recognizes the role of the microbiome in various diseases. As researchers continue to explore these connections, the potential for developing microbiome-targeted therapies grows.
Meanwhile, individuals can take proactive steps by maintaining good oral hygiene and a balanced diet to support gut health. These measures, while simple, could have far-reaching effects on overall health and longevity.
As the research community delves deeper into the mouth-gut-brain connection, the hope is that new, effective treatments for Parkinson’s disease will emerge, offering relief to millions of patients worldwide.