In the early months of the COVID-19 pandemic, researchers at the University of California, San Francisco (UCSF) noticed worrying signs of lingering symptoms in some patients. This was a time when COVID-19 was still largely seen as a transient respiratory virus, and the term “long COVID” had yet to be coined. Clinicians were hearing from young, healthy individuals who reported persistent symptoms such as severe fatigue, respiratory issues, cognitive difficulties, and dizziness long after the acute phase of the virus had passed.
Many of these individuals found themselves unable to perform daily tasks or maintain employment due to incapacitating symptoms. Skepticism from healthcare providers, family, and friends compounded their struggles. However, UCSF clinicians and researchers quickly mobilized, leveraging decades of expertise from HIV research to address this new challenge.
Leveraging HIV Research for Long COVID
UCSF’s rapid response was possible due to its extensive background in studying HIV, a complex virus with long-term effects. This experience allowed them to pivot effectively to studying COVID-19, particularly the long-term symptoms now known as long COVID.
“HIV taught us how chronic viral infections can affect the body long after the initial illness, and how important it is to involve patients in that research,” said Michael Peluso, MD, MHS, an infectious disease researcher and assistant professor of medicine at UCSF.
In March 2020, UCSF launched the Long-term Impact of Infection with Novel Coronavirus (LIINC) program. This initiative has followed over 1,700 participants, collected more than 100,000 biospecimens, and produced significant studies on the disease’s mechanisms. LIINC has also established one of the leading clinical trial programs for long COVID globally.
Insights from HIV Research
Today, over 20 million Americans are diagnosed with long COVID, yet no specific diagnostic tests or treatments have been approved. LIINC co-founder Steven Deeks, MD, began his career during the early days of the AIDS epidemic, which provided critical insights into managing chronic viral infections.
“In the early era of HIV, we tried single-drug therapies, but nothing worked. Two drugs, that didn’t really work. Three drugs – boom,” Deeks said. “That’s the way it worked for HIV, and that may be the way it works for long COVID.”
The UCSF and ZSFG collaboration on AIDS research developed a comprehensive model of care that integrated public health, community organizations, and academic institutions. This model is now being applied to long COVID, fostering partnerships that are beginning to yield answers.
Breakthroughs in Understanding Long COVID
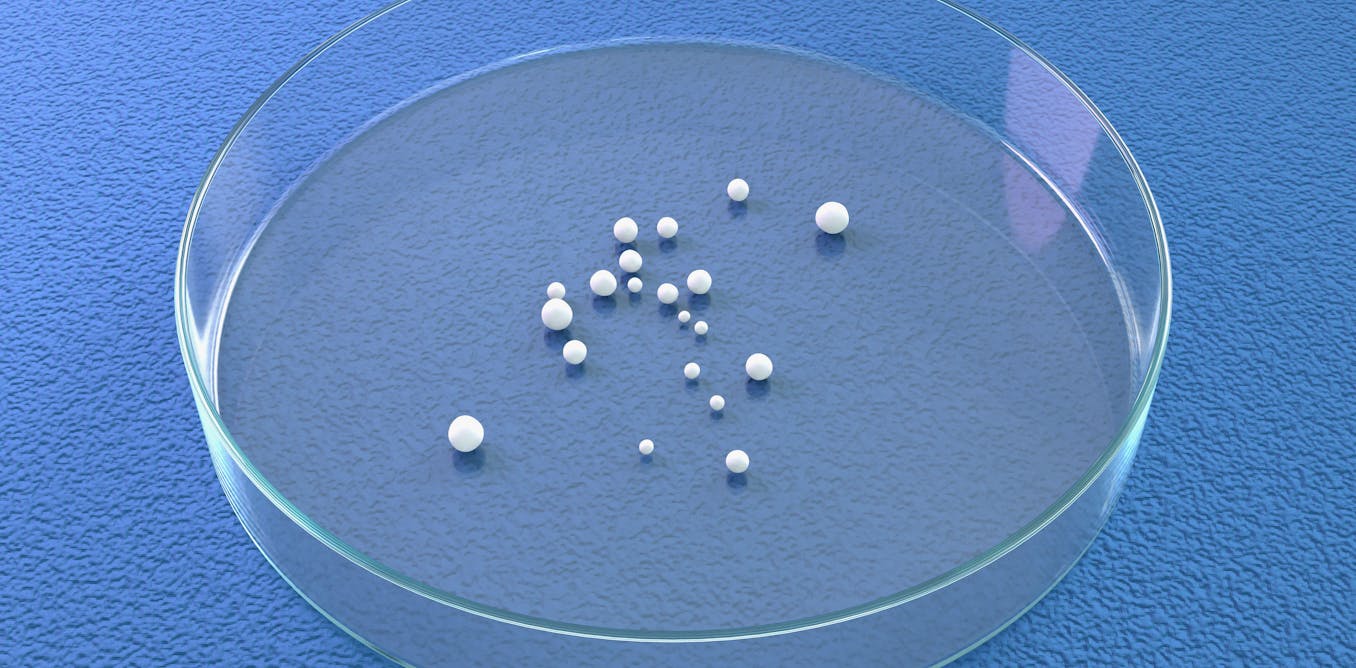
About a year after its inception, LIINC launched the world’s first long COVID tissue bank, discovering that viral remnants could persist in tissues for up to two years. This finding has been pivotal in understanding the disease’s chronic nature.
“Our approach to clinical trials in long COVID is quite similar to our approach to cure HIV,” Peluso explained. “We identify the pathways that we think are driving the problem and use novel therapeutics to target those pathways.”
According to Amy Proal, PhD, president of the PolyBio Research Foundation, UCSF’s foresight in studying long COVID was due to their HIV research background. This allowed them to track long COVID patients effectively and make several breakthrough discoveries.
Ongoing Challenges and Future Directions
While the biological mechanisms of long COVID are not yet fully understood, significant progress has been made. Researchers have identified immunologic differences, abnormal physiologic responses, and viral persistence in various tissues.
“One of the main things we learned is that SARS-CoV-2 is able to persist for a long period of time in various tissues across the body,” said Timothy Henrich, MD, a lead researcher at LIINC.
Despite these advances, more federal funding and investment from the pharmaceutical industry are needed to scale up clinical trials and develop diagnostics. At a roundtable with long COVID experts, Michael Peluso emphasized the need for rapid investment to match the urgency seen during the HIV crisis in the 1990s.
Peluso also highlighted the importance of involving patients in research, a sentiment echoed by Hannah Davis, co-founder of the Patient-Led Research Collaborative. Davis believes LIINC’s work could advance understanding of other chronic conditions, such as ME/CFS and persistent Lyme disease.
“One day soon, we’ll look back on LIINC as part of the groundswell that forever changed the understanding of conditions like long COVID,” Davis said.