Schizophrenia, a complex neuropsychiatric disorder affecting approximately 1% of the global population, is primarily recognized for its hallucinatory and delusional symptoms. However, it also manifests through profound apathy, diminished ability to experience pleasure, and progressive social withdrawal. These “negative” symptoms, for which no effective treatment currently exists, are particularly debilitating.
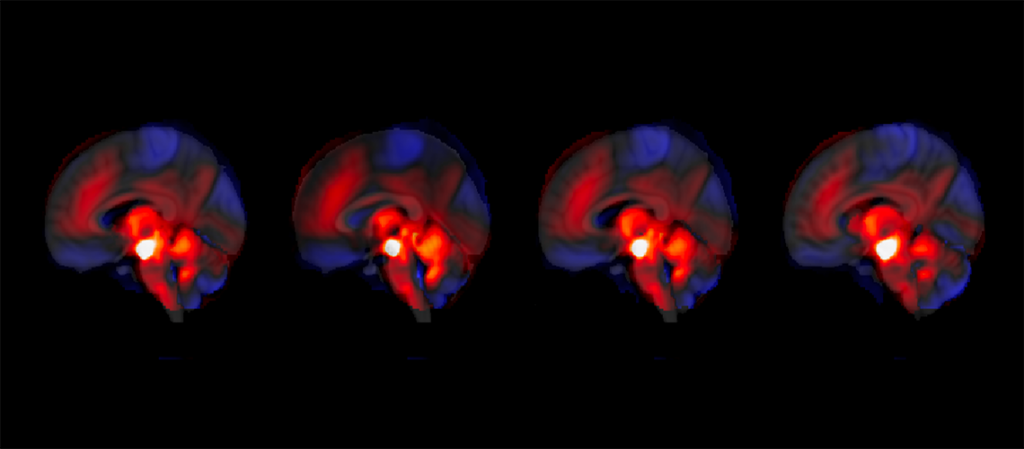
A groundbreaking study by researchers at the University of Geneva (UNIGE) and the Geneva University Hospitals (HUG) has revealed an unexpected role of the cerebellum in regulating these symptoms. The study shows that stronger cerebellar regulation of the brain’s reward system correlates with a reduction in negative symptoms, while weaker regulation is linked to an increase in these symptoms.
The Cerebellum: A Hidden Regulator
Traditionally viewed as a region primarily responsible for motor functions, the cerebellum is now being recognized for its significant emotional and cognitive roles. “What is sometimes called our ‘little brain’ actually contains 50% of all our neurons,” explains Indrit Bègue, assistant professor at the UNIGE Faculty of Medicine and lead researcher of the study. This innovative research highlights the cerebellum’s influence on the ventral tegmental area (VTA), a key component of the brain’s reward system.
Abnormalities in the VTA, particularly its overactivity, have been associated with the negative symptoms of schizophrenia. This overactivity leads to a blunted perception of salience, where “everything feels the same,” resulting in a lack of motivation. The study’s findings suggest that the cerebellum plays a crucial role in modulating this mechanism.
Breakthrough Research Findings
The research team followed 146 patients over a period of 3 to 9 months, analyzing an independent validation cohort to observe the functional connection between the cerebellum and the VTA in the context of schizophrenia. “We show that stronger cerebellar regulation of the reward system is associated with a reduction in negative symptoms — and conversely, weaker regulation with an increase in symptoms,” notes Jade Awada, a doctoral student and first author of the study.
The analyses were conducted by Awada and Farnaz Delavari, co-first author and researcher in Professor Stephan Eliez’s laboratory. Their work provides a new understanding of the cerebellum’s role in schizophrenia, offering potential pathways for targeted therapeutic interventions.
Implications for Future Treatments
The discovery of the cerebellum’s involvement in regulating the reward system opens up promising avenues for developing treatments targeting these negative symptoms. “This newly identified mechanism could lead to the development of therapies that specifically enhance cerebellar regulation to alleviate negative symptoms,” suggests Bègue.
By the Numbers: Schizophrenia affects approximately 1% of the population globally, with negative symptoms significantly impacting quality of life.
While current treatments for schizophrenia primarily address positive symptoms such as hallucinations and delusions, the lack of effective interventions for negative symptoms remains a significant challenge. This study’s findings could shift the focus of future research and treatment development.
Looking Forward
The implications of this study extend beyond schizophrenia, potentially informing research into other neuropsychiatric disorders where the cerebellum might play a role. As researchers continue to explore the cerebellum’s functions, new therapeutic strategies could emerge, benefiting a broader range of conditions.
Meanwhile, the team at UNIGE and HUG plans to further investigate the cerebellum’s regulatory mechanisms and explore potential clinical applications. As this research progresses, it holds the promise of transforming the treatment landscape for schizophrenia and improving the lives of those affected by the disorder.