A pioneering study led by Weill Cornell Medicine and NewYork-Presbyterian reveals that whole-genome sequencing could significantly improve the identification of patients who would benefit from PARP inhibitor cancer treatments. This innovative approach, detailed in the January 12 issue of Communications Medicine, shows promise over existing commercial methods, suggesting a potential shift in cancer treatment protocols.
The research involved a comprehensive analysis of hundreds of tumor samples, obtained with informed consent, as part of a precision medicine initiative by Weill Cornell, NewYork-Presbyterian, and Illumina, Inc., a leading biotechnology firm specializing in DNA sequencing. The study’s findings indicate that further development of this method is warranted.
Revolutionizing Cancer Treatment with Genomic Insights
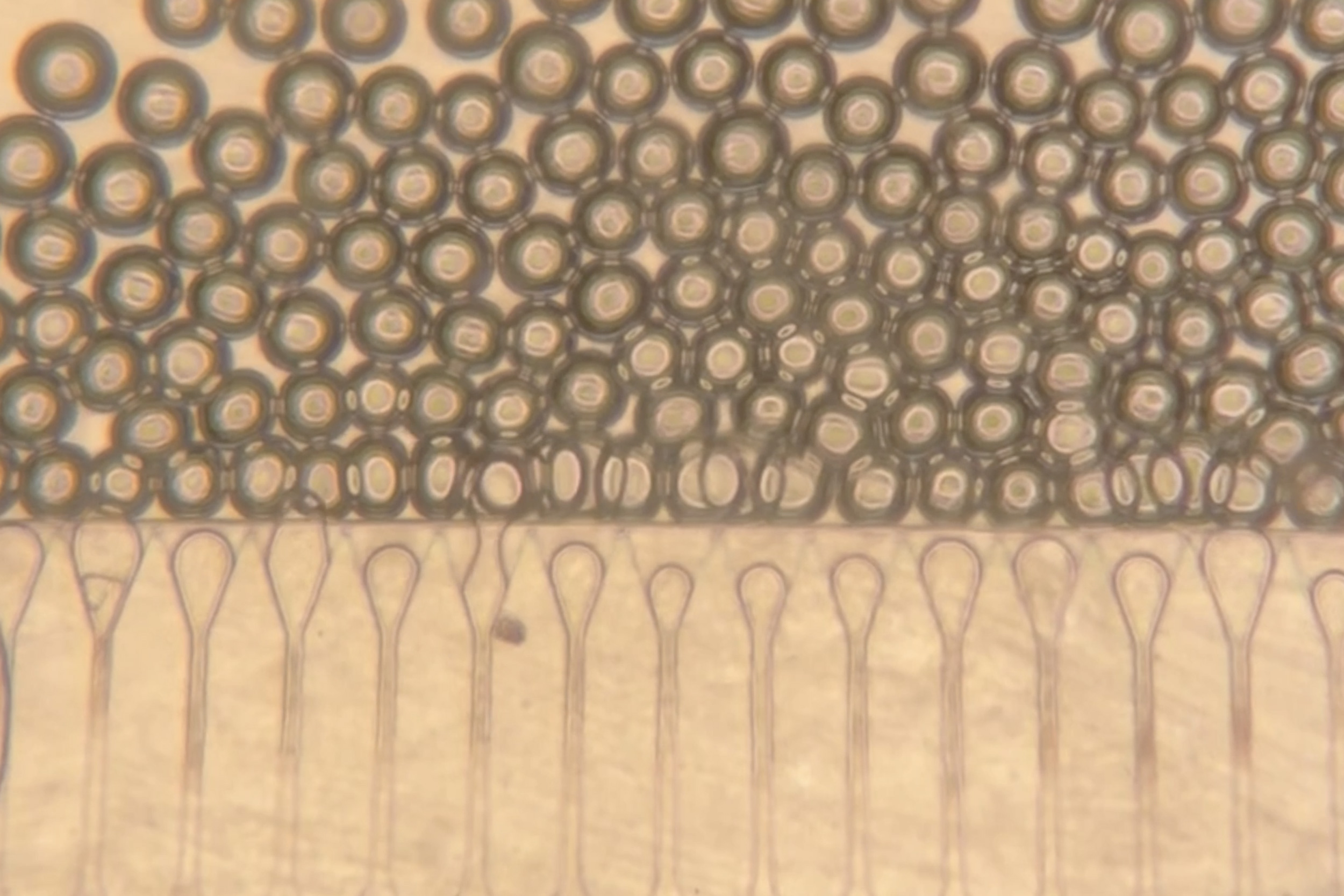
The study’s authors performed whole-genome sequencing to train and validate an algorithm capable of detecting homologous recombination deficiency (HRD), a DNA-repair defect that makes tumors susceptible to PARP inhibitors. These inhibitors disrupt DNA repair, causing cancer cells to accumulate damage and ultimately die. The research suggests that this algorithm is more accurate in predicting treatment responses than current methods.
“A comprehensive analysis of the entire genome has advantages compared with traditional, targeted detection strategies for predicting homologous recombination deficiency,” said Dr. Juan Miguel Mosquera, senior author of the study and professor of pathology and laboratory medicine at Weill Cornell.
This collaboration with the medical diagnostics company Isabl, Inc., marks a significant advancement in precision medicine, potentially expanding the scope of patients who can benefit from targeted cancer therapies.
Beyond BRCA: Expanding the Genetic Horizon
Traditionally, clinicians have focused on BRCA1 and BRCA2 mutations to determine patient eligibility for PARP inhibitors. These mutations are prevalent in breast, ovarian, pancreatic, and prostate cancers. However, recent research indicates that numerous other gene mutations can also impair DNA repair processes. Whole-genome sequencing, now more affordable, offers a broader detection capability.
The study utilized 305 samples from patients at Weill Cornell and NewYork-Presbyterian to train the algorithm developed by Isabl. The algorithm was then validated on a cohort of 556 cancers and tested against commercial methods with an additional 212 tumor samples.
By the Numbers: The algorithm identified DNA-repair deficiencies in 21% of breast tumors, 20% of pancreatic and bile duct tumors, and 17% of gynecological tumors. Crucially, 24% of these cases did not involve BRCA1 or BRCA2 mutations.
Implications for Future Cancer Treatments
The findings underscore the potential for whole-genome sequencing to transform cancer treatment by identifying a wider array of genetic mutations. This could lead to more personalized and effective treatment strategies, reducing reliance on traditional methods that may overlook critical genetic information.
In several instances, the algorithm corrected “false negative” and “false positive” predictions from commercial methods, aligning more closely with actual patient outcomes. This accuracy could enhance clinical decision-making and improve patient prognoses.
Looking ahead, the research team plans to conduct larger studies to further validate the algorithm’s efficacy as a general tool for guiding cancer treatment. This could pave the way for its integration into standard clinical practice, offering hope to patients with diverse genetic profiles.
As the field of genomics continues to evolve, the integration of whole-genome sequencing into cancer treatment protocols represents a significant leap forward. The potential to identify previously undetectable genetic mutations could revolutionize patient care and improve outcomes across a range of cancers.